If you are in pain and want to explore pudendal neuralgia treatment options, call Dr. Attaman’s Seattle office (206-395-4422) or Bellevue, WA office (425-247-3359), or email us to schedule an appointment.
It is amazing how many causes of chronic pelvic pain there are; infection, endometriosis, pelvic muscle imbalances, gastrointestinal causes, joint pathology, etc. There are literally dozens of causes of chronic pain in this region.
One of the rarer causes of chronic pelvic and genital pain is a disease called Pudendal Neuralgia. I have treated many patients over the past few years with this diagnosis, and it has been professionally rewarding for me.
“Pudendal neuralgia is a commonly overlooked condition when evaluating chronic pelvic and genital pain disorders. The
pain associated with many of the following disorders may be caused by (or in part by) pudendal neuralgia or pudendal nerve entrapment: vulvodynia, vulvar vestibulitis, interstitial cystitis, irritable bowel syndrome, chronic or non-bacterial prostatitis, prostadynia, burning scrotal syndrome, chronic pelvic pain syndrome, proctalgia fugax, hemorrhoids, coccydynia, piriformis syndrome, anorectal neuralgia, pelvic congestion, pelvic floor dysfunction, ischial bursitis, levator ani syndrome, and others. All of these disorders can have the same symptoms as pudendal neuralgia or actually be caused by PN. Sadly, it is common for patients with any of these conditions to be told their problem is psychosomatic and to seek psychiatric help.” — Health Organization for Pudendal Education
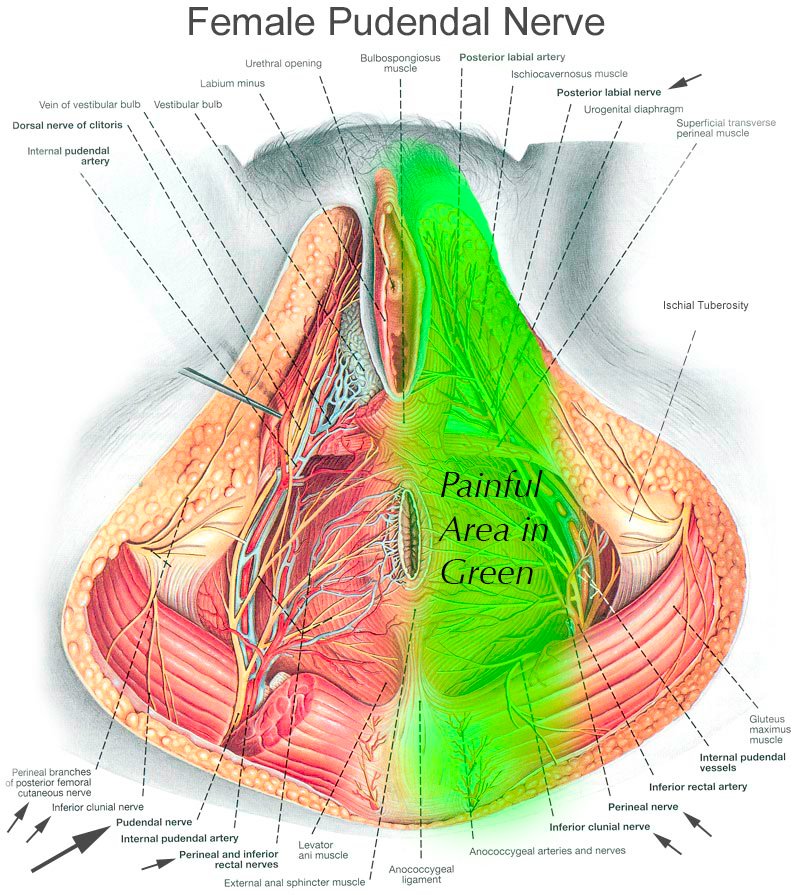
The pudendal nerve is a very little known but very important nerve in the pelvis. It is a nerve that provides sensation to your inner buttocks, anus, perineum (the area between your anus and genitalia), and genitals. This nerve can be injured or irritated for many reasons. In roughly 50% of patients, we have no idea what triggered the issue. Some patients have Pudendal neuralgia from falling on their buttocks while snowboarding. It can be as simple as that. Some patients have endured serious surgeries such as pelvic sling mesh placement and have woken up with this pain. Regardless of the cause, the symptoms can be severely debilitating.
Typically my female patients with pudendal neuralgia experience severe perineal burning electrical pain and pain around the genitals, especially the vulva and the clitoris. They often complain of a sensation of “sitting on a rock” near their sitting bones (ischial tuberosities).
Men with pudendal neuralgia typically have pain more focused around the scrotum or end of the penis. The most common cause in men by far is extreme bicycling.
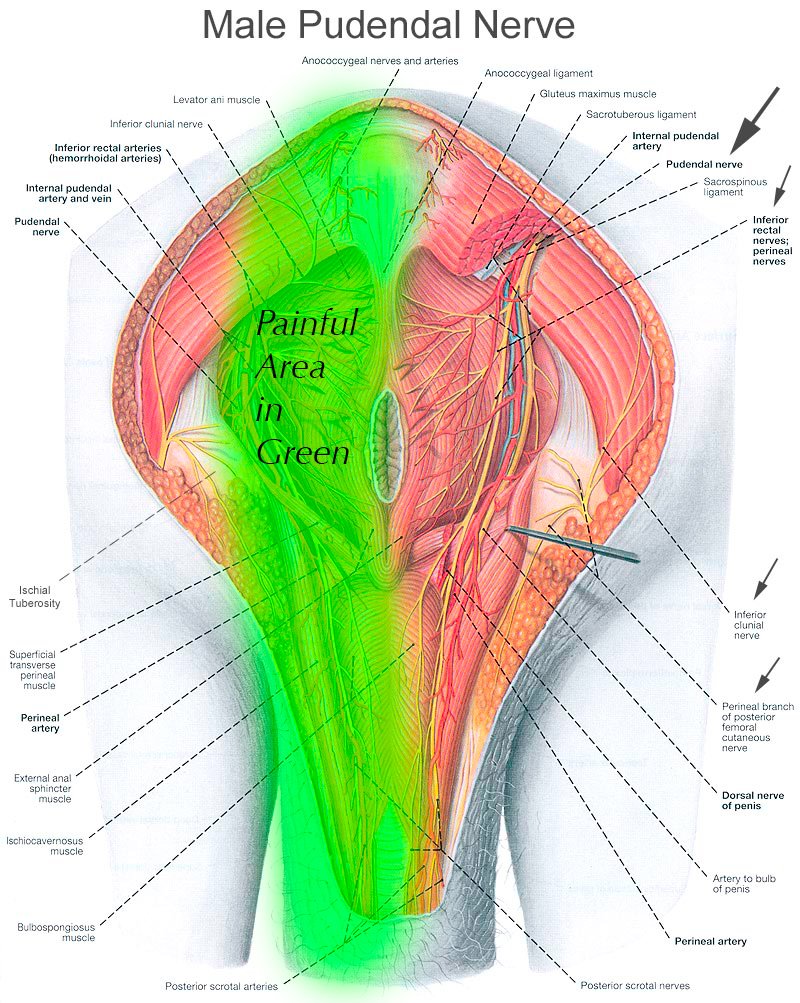
The images you see demonstrate the course of the pudendal nerve, and you can imagine that burning, electrical, stinging pain anywhere along this nerve would be extremely distressing.
The first step in beating pudendal neuralgia is education. This means finding physicians that are versed in this nerve. Unfortunately, there are very few of us. This seems to be due to the fact that we are not taught about the pudendal nerve in medical school, residency, or even fellowship training. Indeed, I’ve spoken to urologists and gynecologists who either had forgotten about this nerve or had no idea it can play a role in chronic pain. Even though I completed a very intensive Pain Medicine fellowship, I never learned of it either. It was not until I started seeing patients in my clinic for whom nobody had found a diagnosis that I did further research and came to appreciate the importance of this nerve.
I’d strongly recommend you visit www.pudendalhope.info to get educated on this condition. It is a wonderful resource for education and resources.
You can read an interview I granted with www.pudendalhope.info about spinal cord stimulation (SCS) for Pudendal Neuralgia. You can click on the following link to read my interview: Interview with Dr. Attaman by pudendalhope.info
The next step is getting diagnosed and treated. Typically, this means seeing a urologist, uro-gynecologist, or OB/GYN specialist who likes to treat pelvic pain. One such person I can highly recommend in my state of Washington is Dr. Cindy Mosbrucker. If it is found that your pain is not due to issues with your internal organs, then the pain may be due to pudendal neuralgia. This is when I can help.
Typically I will review your records from the other specialists you have seen to be sure no diagnosis has been overlooked. I review any tests such as MRIs you may have had. I then perform a very careful history and gentle physical exam. We then discuss treatment options.
The treatment options are generally “multi-modal,” which means it would involve referral to various specialists with unique skills in treating this issue, such as physical therapists who work on the pelvic floor. Medications such as custom made suppositories to relax your pelvic nerves and muscles may be prescribed. Special Imaging studies such as MRI neurogram of the pudendal nerves may be ordered. Typically, I will want to confirm your Pudendal nerves are causing your pain by using an ultrasound machine to see the nerves and guide a thin needle to them through your buttocks and turn them off temporarily via a local anesthetic injection. This is called an ultrasound-guided pudendal nerve block. Oftentimes the treatment just detailed is sufficient to cure the issue. If insufficient, you may be a candidate for other procedures I perform such as low volume caudal epidural injections, pulsed radiofrequency ablation of the pudendal nerves, botox injections into the pelvic floor muscles, or spinal cord stimulation trial over a special area of the spinal cord called the conus meddularis.
Pudendal Neuralgia is a challenging condition to treat and diagnose, but there is certainly hope!
I am one of the few physicians in the world to routinely perform pulsed radiofrequency treatment of the pudendal nerve. It is a technically challenging procedure and time consuming. As I have performed many of them I have become proficient in this procedure and it is available to patients who are not responding to more conservative measures. Some literature on this procedure is below:
Pudendal Neuralgia FAQ
How do the symptoms differ in women vs. in men?
In women, the pain is commonly in the perineum and vulva. In men, the pain is more common in the perineum and glans penis (tip of the penis).
What conditions can pudendal neuralgia be mistaken for?
Unfortunately, pudendal neuralgia symptoms are mirrored by many, many other diseases and syndromes. Almost always, other disease states need to be “ruled out” prior to pursuing a diagnosis of pudendal neuralgia. In women, endometriosis, vaginitis, UTI, vaginismus, or other infections need to be ruled out. In men, prostatitis and bladder issues need to be ruled out. I always encourage my female patients to be fully evaluated by a gynecologist or urogynecologist prior to seeing me if they have genital pain. They should also see a colorectal surgeon if there is severe rectal pain. My male patients should be evaluated by a urologist if they have genital pain. They should also see a colorectal surgeon if there is severe rectal pain.
I would estimate that 90% of the patients I see in my clinic who are later conclusively proven to have pudendal neuralgia have been misdiagnosed by multiple prior physicians. I have seen many women sterilized (had a historectomy) for this condition. I have seen many women have many invasive surgeries and long courses of antibiotics for this condition. Unfortunately this worsens the underlying problem.
Almost 100% of the men I see have been misdiagnosed with “prostatitis,” in the past, and had multiple courses of antibiotics.
What causes it?
In roughly 50% of cases, there is no known cause in women and men. In women, the most common known causes are pelvic floor surgeries by far, particularly pelvic mesh placement. In men, the most common known cause is trauma, in particular bicycling, falling on the buttocks during skiing or snowboarding, or violent masturbation.
To what extent can it be prevented?
Avoid extreme bicycling, avoid pelvic sling/mesh placement if possible.
What are the risk factors?
See causes, above.
Is it hereditary?
Not to our knowledge. I have never had a patient mention pudendal neuralgia was present in any other family member.
Can pudendal neuralgia be treated?
Yes, there are many treatments!
Can it just go away by itself?
Yes, absolutely. However the longer you live with it, the less likely it is to go away by itself.
What are the treatment options?
The most conservative treatments include lifestyle modification, such as cessation of extreme bicycling. Other conservative options include pelvic floor physical therapy, in which a physical therapist places their fingers through the vagina and or rectum to stretch contracted pelvic floor muscles. Then medications can come into play, such has specially prepared vaginal or rectal suppositories with medications such as valium and baclofen which can help relax muscles and nerves in the pelvic floor. Oral medications such as muscle relaxants and nerve pain medications come next. Finally, invasive injection procedures enter the picture if needed. Such procedures include image-guided pudendal nerve blocks to diagnose the condition and hopefully gain some long term pain relief, image-guided pudendal nerve pulsed radiofrequency treatment, and image-guided botox injections of the obturator internus muscle to reduce pressure on the pudendal nerve as it passes through Alcock’s canal
We also are the only clinic in the pacific northwest to perform cryoablation treatment to the pudendal nerve, in which a special machine is used to create an ice ball at the tip of a specialized needle. This ice ball literally freezes the pudendal nerve, and interrupts the pain signals on a long term basis. The nerve grows back unharmed after 6-12 months, but oftentimes the pain does not return with it. This is a neurodestructive treatment, and therefore not a treatment we utilize unless necessary. We operate the “gold-standard” machine used for cryoablation, the EpiMed PainBlocker. You can learn more about this device by clicking here. You can also watch an outstanding lecture about cryoablation from the doyenne of this modality and outstanding Pain Medicine physician, Dr. Andrea Trescot, here. Dr. Trescot’s practice is in Alaska and can be contacted here.
Finally, the most invasive treatment I offer is called spinal cord stimulation, in which a special wire is placed along the spinal cord in the spine, and a small electrical current is applied to it. This blocks the pain signal from the pelvis to the brain. I use conventional spinal cord stimulator systems, as well as the newly released and very advanced St. Jude/Abbot DRG (dorsal root ganglion) stimulator, in which I can place these wires upon the S2-S4 nerve roots which form the pudendal nerve. This is a very powerful, expensive treatment, but one involving minor surgery, and thus I try save this option for last. You can read more about spinal cord stimulation in an interview I did with PudendalHope.
You can read about the St. Jude DRG stimulator here:
https://www.neuromodulation.abbott/us/en/chronic-pain.html
Oftentimes, particularly for patients traveling from foreign countries to see me, I will combine many of the procedures above in a single treatment. Therefore a patient may have pulsed radiofrequency treatement to the pudendal nerve, pulsed radiofrequency treatment of the pudendal nerve, and botox to the obturator internus muscles all in one session. The helps minimize the need to travel to my clinic multiple times to receive these treatments individually.
How does treatment work?
See above.
How long does the treatment take?
I treat nerve pain of all sorts all over the body. I want to be frank and state that pudendal neuralgia is one of the toughest to beat. Typically, treatment takes many months, when incorporating pelvic floor physical therapy, medications, injections, and lifestyle modifications. Patients typically will start with at least two diagnostic image-guided pudendal nerve blocks to confirm the diagnosis. They may then need to proceed to more advanced procedures such as pulsed radiofrequency treatement, botox, or in some cases spinal cord stimulation or dorsal root ganglion stimulation. Finally, surgical intervention may be needed in some cases.
Is there anyone who should not undergo treatment?
No, there is a treatment option of some sort for everybody.
What if I’m pregnant?
If you are pregnant, you are only eligible for pelvic floor physical therapy and lifestyle modification. I do not offer injection or medication treatments for pregnant patients.
That said, I have never met a pregnant patient with chronicpudendal neuralgia. If they do have it, it is very transient.
How should I prepare for treatment so it goes smoothly?
We have specific instructions to help get the most out of your treatments, and these are provided to you as you enroll.
Can you walk me through what happens on treatment day?
For an injection, typically you will arrive at my clinic for check in. We will then discuss the procedure and answer all your questions and obtain written consent from you. We then perform various injecitons as described above, almost all of which involve using an ultrasound or x-ray machine to very precisely guide a very thin needle through the skin of your buttock to the pudendal nerve, obturator internus muscle, or sacrotuberous ligament. In general, I can do all procedures through a single needle poke, as I can redirect the needle deeper in your body to various targets. The injections last anywhere from 5 minutes to 45 minutes depending on which injection(s) you will receive. You are then sent home with a driver.
Do I need multiple visits?
Typically, yes, multiple injections are needed, but not always.
What aftercare do I need to do?
We have special protocols for you to follow depending on the treatment you are receiving.
What are signs of a smooth recovery?
Gradual reduction or elimination in your pain, however the pain typically fluctuates up and down for the first few weeks after treatment, so do not expect your pain to go away immediately.
How can I prevent it from returning?
See above.
How much does the treatment cost?
Treatment cost is often covered by insurance. Many procedure however are not covered by any insurance, and therefore need to be paid directly by you. Costs range from $300 to $3000 per side, depending on the complexity of the procedure performed.
How can I find local help?
Unfortunately, rarely. There are very few physicians that treat pudendal neuralgia in the entire world. This is truly unfortunate. I would suggest you visit pudendalhope.info for local physicians that may help you.
How do I know whether a given doctor can actually help me?
Ask them how many patients with pudendal neuralgia they have treated in their career. If it is less than 10, it is unlikely they have the expertise to help you. Unfortunely, 99.9% of physicians have never (knowingly) seen a single case of pudendal neuralgia.

Can you PLEASE recommend anyone in Western North Carolina (Asheville area) with your specialty in Pudendal Neuralgia?
Pain started shortly (6 Months) after knee surgery. I have seen my GP numerous times. Been to two lower pelvic physical therapy groups of sessions. Seen 3 Neurologists with nerve conduction studies with no results. I have seen a urologist twice. I have had a colonoscopy with perfect results. And I have had an MRI (standard) which showed no abnormalities. I recently had a nerve block to the Pudendal nerve under the coccyx area which was unsuccessful. I am male, 72, in relatively good physical health with BMI of 25. Walk 2 or more miles 2 or more times a week.
Symptoms are Sitz bones and Anal pain when sitting. Gets worse throughout the day. Most of pain goes away on standing or when on a toilet seat. No pain while sleeping. Typical Pudendal Neuralgia symptoms. Most of the Pain Management specialists want to only recommend addictive drugs. I don’t know where to go next.
I am very sorry but I do not know anybody in your area. There are unfortunately very few physicians in this country that deal with this condition. Please refer to the doctor listing at http://www.pudendalhope.info
http://pudendalhope.info/node/58#MA
Best, Dr. Attaman
Hi there,
My fiance has been seeing Sarah Talley at Carolina Pelvic Health Center in Raleigh, NC. She is amazing and is a Physical Therapist who specializes in Pudenal Neuralgia and pelvic pain.
Here is her contact information: http://www.carolinapelvichealth.com/
We are in Charlotte and this is the closest specialist we could find to us.
Wishing you all the very best!!
Brandi
Thank you for the useful information. I hope this helps out other folks in your area! Dr. Attaman
I am a male in your area who has suffered from CPPS for over 25 years. I have tried all the antibiotics, painkillers, etc. and the only way I find relief is applying ice to the pelvic area when sitting. Is there any hope for me?
Dear Tom,
Of course! There are almost always options for this condition. Dr. Attaman
Hello Anon,
Dr. Evans at Wake Forest Urology is very familiar with PN/PNE. I used to travel to see him from SC for treatment. I was able to overcome my pain of several years for almost a year and unfortunately had a re-injury again.
You can get help but it does take a lot of patience.
Best of luck to you. If you find someone else that helps nearby I would love to know. I’m considering creating an account on the pudendal hope site. It is full of great material.
You might want to look into getting a MRI of the sacral. I have these exact symptoms and thought it was endo then they thought I had pudendal neuralgia and I finally after 10 figured out my problem was Tarlov cysts on my spinal cord. After 10 long years I finally have a diagnosis to all my pain. Not a good diagnosis but it is a diagnosis.
What symptoms did you have. I have a tarlov cyst and have been having issues. Any help would be great
hi i have been living with symptoms close to 90% of those describe by pudendal nerve syndrome and pudendal neuralgia. i have rule out so many other factors from testicular ultrasounds to std nothing was found no one knows what I’m feeling or trying to explain. I’ve been doing research on my own for months now and finally i have came across this condition which sorry to say yet feels rewarding to at least feel like I’m not going crazy i resigned in new jersey is there any physician in my area that might can help me if not what kind of physician would be suitable for me to see ?
Also i the process of ruling out situations i also was told i have a chronic tear in my groin region I’m assuming it has been there for a while and i didn’t know about it i just want to know can this be a reason for PNS or PA or PNE ?
ps after further and extensive research in reading i found out about this diagnosis after looking into the blood vessels in the ingunial region
please help me :(
Dear J.W.,
I’m sorry to hear of your situation. I’m not sure of anybody that deals with pudendal neuralgia in NJ. Have you looked at the pudendalhope.info physician finder at: http://pudendalhope.info/node/58#NJ? Kind Regards, Dr. Attaman
I’m only 33 is these diagnosis seen at my age
Yes unfortunately pudendal neuralgia is fairly common in your age group. I cannot confirm your specific diagnosis however. All the best, Dr. Attaman
Yes, unfortunately for men it seems late 20’s to early 40’s is the most common age to experience pudendal neuralgia. Dr. Attaman
I am female Dx’d with PN via specilist (not practicing now) in AZ.. He had offered ablation of PN under CT guidance. Can it be done without CT? Considering the neurostimulaor by surgeon in CA. Never had an MRN. There is suspected rectal nerve damage as well, all from pelvic surgeries for SUI and POP. I am living a nightmare. Have no quality of life. Botox is at best a temporary and very expensie bsnd-aid. Already had mutiple mesh removal surgeries by the best mesh complication surgeon in CA. Meds just take the edge off and have horrible side effects. Pease help.
Dear V,
I’m sorry to hear of your problems. It can be done without CT but doing it under CT is a good idea. I cannot give you specific medical advice, but in general, other options may include spinal cord stimulation or pulsed radiofrequency treatment of the pudendal nerves. You can read an interview I did with the pudendalhope.info website on spinal cord stimulation for pudendal neuralgia here: http://www.pudendalhope.info/node/22
Hi, I have had PN for 9 years. Tried all the systemic meds- can’t tolerate them. Had bi-lateral pn decompression surgery 3 years ago – no change in pain. I apply xylocaine ointment every hr when awake. I have to pay for most of it at full cost. Pain clinic thinks 15g a day is too much to use, but without it I am in extreme pain. Never had side-effects from it. Has anyone applying xylocaine 5% for a non-vanity reason had a problem with high blood toxicity levels?. My test showed an almost trace amount in bloodstream. Cheers
Dear Sarah,
I have not had a patient in my practice using this medication as often as you are. It is good to hear you have had no side effects. I think your pain clinic is wise in advising you to reduce your dosage. Have you tried spinal cord stimulation at the conus medullaris for this condition? Kind Regards, Dr. Attaman
Due to an obgyn oncologic condition, I had to have an inner vulvectomy. I have healed but it is apparent that the left pudendal nerve was damaged either from the pre surgical block but most likely due to the deep stitching that was required. Can you recommend a physician trained in oregon? I expect it will require a radio frequency ablation.
Thank you
Dear Chandra,
Unfortunately I am not aware of anybody in Oregon who treats this condition. I do have many patients travel to Seattle to see me from Oregon however. Kind Regards, Dr. Attaman
Hey there, I believe I may be dealing with this disorder. I have occasional penile tingling and burning along with areas in my pelvic floor region having the same deal. It goes on and off. But is worrisome being a 19 years old guy. I just want to have a family of my own one day and be able to have sex for as long as possible. Would you recommend taking Acetyl-L-Caroline and lipoid acid? I’ve read that those two can help with nerve pain and healing. And Also, I like in NW Iowa not too far from Minneaoplis or Mayo clinic. Do those location offer and step to combating this?
Dear Michael,
I’m sorry to hear you are suffering. I cannot dispense medical advice in this format. I would suggest you visit the Urologists and Pain Management specialists at Mayo Clinic.
Kind Regards, Dr. Attaman
Nobody at University of Iowa Hospials and Clinics treats this.
Who would you recommend in the Midwest?
Thank you so much!
Unfortunately, I am not aware of any pain physicians in your area. I wish there were many such people so patients would not need to fly from around the country to see me. Kind Regards, Dr. Attaman
Hi,
I am dealing with PN for almost 9 months. All my symptoms are in my penis. I have pain, burning sensation and some numbness. I tried nerve blocks and I am all the time on 1800 mg Gabapentinum.
Now I am thinking seriously about neurostimulation. Do You think I am good candidate for that treatment option? Does it make my penis completely numb because of electric impuls or it take away only pain?
Thank You very much.
Can you recommend a doctor in central florida who specializes in pudendal nerve problems?? I also need one in Connecticut as we are snowbirds. Thank you. A lot of gyn doctors have no clue what this nerve does
Possible pudendal nerve problem
I am a healthy 71 year old male, with a history of BPH problems, and also a large hydrocele that may be making my diagnosis more difficult.
I originally thought I developed a UTI and started treating it with some old cipro I had. I then took a nine hour automobile drive, and had difficulty getting comfortable in my scrotal area. Initial symptoms were a tender urethra, and sensitivity and soreness in the scrotal and perineal areas near the right buttock. It was uncomfortable to sit, except on the toilet, and pain was relieved when standing or lying down. Pain was never sharp, but more of a soreness and maybe a two out of ten.
My doctor suggested I try prednisone and some PT. Six hours after my first dose of prednisone I had substantial relief. The PT produced no immediate results. It has been over a week now, and there has been no further relief than that from the original prednisone dose. I still have the tender urethra (during urination only). My pain (more of an annoyance) is centered in the crease area between my right thigh and perineum. Sitting is still uncomfortable, except on a toilet seat, and standing and lying are fine. A coccyx cushion does not work unless I center the gap under the pressure point in my right thigh area. Thus far, I have not experience the sharp pains expressed by others, and as of now it is just an annoyance.
My question is: do I have a pudendal nerve problem, or could it be a UTI or a complication from the hydrocele or something else? Where should I go from here, and what else should I try to help my diagnosis? Thank you.
Can you recommend doctors and Physical Therapist in Houston. I have tried the PN page but I must say that lady Feetima on there is out of touch with PN.
I had an MRI 3t for PN and the doctor said I had it then with the test he said not. I have not had any pelvic floor surgeries. I really need a diagnoses so I know what to do. I have tried 6 months of Pt with two different PT’s and no better, acutally the nerve pain has moved and now I have it in my feet, my hands and all over. I wondered someone here L4 and S1 are issues, which I had checked out and there is an issue at my L4 with spine. I have lumbarsacral tranisitional vertabre and so they say to move everything up notch. Sorry for rambling but on the side that causes issues my thigh goes numb a lot, but only to me knee.
I saw where you shoot the Alcock Canal and was wondering since mine is all rectal maybe I should get a marcaine injection into that area.
I can’t believe in Houston TX where there is a hospital on every corner I cannot find someone to help.
i have most of these symptoms with the addition of significant coccyx pain which arose immediately subsequent to a traumatic caudal epidural. Would like to know if you have encountered any other patients with history of injury post caudal epidural. And of course whether such a nerve injury, from needle trauma, is treatable. I have had this pain since 1987, and as bad as it was initially, it is much worse now.
Dear Janet,
I have never heard of this happening after a caudal epidural injection. I have performed hundreds of caudal injections myself. However, if image guidance was NOT used for your caudal, there is a possibility pudendal nerve injury could have occurred as the pudendal nerves are in the general vicinity of the sacral hiatus where the caudal epidural is targeted. Kind Regards, Dr. Attaman
After numerous tests my mother has been diagnosed with PN. We cannot get her into the pain clinic until mid October and she is miserable. I am not sure of the suppository that was prescribed but never-the-less my mother went to fill the order at the pharmacy and it was $220.00 for two weeks. She is on Medicare and cannot afford this at ALL. Any suggestions for a cheaper suppository? Mom is not herself the past few months and this is very sad for our family.
This all started about 20 years ago she was walking to the cabin from fishing, her left leg fell in a hole with a large pipe inside hitting her tail bone area. Now the result of this fall is starting to rear its ugly head.
Summary: Cheaper suppositories that Medicare might cover.
Also, my mother seems to have more problems and pain from PN in the summer. Not sure if you found this to be a commonality among patients.
I’ve had PN for 9 yrs. I believe I got this from an endometrial ablation, the one where they fill you with hot water. The side effects state”nerve damage possible”. Have you ever heard of a patient’s nerves affected by ablations?
I have an MRN, which I know aren’t super dependable, show damage to the perineal nerve. My pain is extreme w/sitting and goes from my Ischial tuberosity towards my anus and then down my hamstring.
Also, do you have any programs for out of state patients?
Hello,
Yes, I see many out of state patients. Please feel free to call my office for a consultation appointment. We can do the initial consultation over phone or video chat such as Skype, etc.
Kind Regards, Dr. Attaman
Could you please refer me to someone who specializes in PN/Pelvic Pain? I’ve been having problems ever since my hysterectomy on February. I’ve been to numerous doctors and pelvic floor therapy. I had to have another surgery recently to remove left ovarian mass thought that was going to cure the problem of pain on left side clitoral and labia.
I would recommend Dr. Todd Lininger, MD in West Bloomfield, Michigan. He is the best pain doctor in the state. Dr. Attaman
I live in michigan. Thank you.
I have been to many doctors and PTs over the past 4 years with no relief – are you able to recommend someone that specializes in this in the Chicago area?
I am not aware of anybody in Chicago that specializes in this nerve. You could check the list of physicains at pudendalhope.org for more information. Best Regards, Dr. Attaman
I’m a female and thought I’d pinched a nerve doing a 100 mile ride. I learned later that the support rails were slightly bent such that one side was a bit higher than the other. By the time I got home from the ride it was pretty excruciating to try to sit on the saddle (I had to stop a lot, which I never do). Since then it’s sort of progressed and my right buttock gets pretty achy after sitting for an hour or so, even on a couch (and rides are still a problem, even with a new saddle and much more upright position). I just started PT and the therapist mentioned I might need to have the pudendal nerve checked if 4 wks of PT doesn’t help. Since I likely know when I injured whatever is going on, I’m curious as to whether it might eventually resolve on its own if it is indeed the pudendal nerve? It’s been since July, but I’m still riding (although down to one day a week, 2 1/2 hrs). Thanks-good info.
Dear Lynne,
I’m sorry to hear of your problems. Pudendal neuralgia can indeed resolve on its own, but I recommend aggressive treatment early on. Kind Regards, Dr. Attaman
I have had xrays mri no abnormality. Symptoms are back pelvic pain buttocks severe pain numbness groin and vulva area. Sensation leg hard to describe tingling burning. I think this could be peudenal nerve but do not know who to go to near where i live which would be johnstown pittsburgh pa area. Your help would be appreciated.
Hello,
There are so many things that can cause this type of pain. Unfortunately I do not know of anybody in your area, but you might want to check http://www.pudendalhope.org for resources. I see patients from around the country as well. Best Regards, Dr. Attaman
It was great to find your blog. I have been to so many specialist and it is amazing that they do not know about PN (they all try and correct me when I ask about Pudendal with “you mean the Perineal Nerve”). OHSU Center for Pain Management (Portland Oregon) diagnosed me and was going to do cyroneurolysis but my Insurance has changed and I have been looking for a Doctor ever sense. I’m to the point of possibly paying out of pocket for treatment. The Doctor from OHSU did not talk to me about treatment options, just scheduled me to have the actual cyro treatment done (from a different Dr which I would meet day of treatment) and I would like to speak to someone in the field of PN.
I have had a total of 5 surgeries with the last two dealing with the total removal of mesh which had grown into my urethra and reconstructive surgery of my pelvic floor (done at UCLA).
Not sure if you have a list of Doctors for the NW, but could sure use some help. There seem to be Doctors that may diagnosis PN, but from what I have found really don’t treat or even have a great knowledge of the nerve or treatments.
PT has been the biggest help, but we can’t get past all the tightness form my SI and PFD that make it hard to focus on my PN.
With each passing year of my pelvic pain and nerve damage, chronic pain, urinary and bowel problems, depression and anxiety, SI joint, and my PN pain I’m feeling like I’m going to jump out of my skin – this is not living. I keep thinking next year I’ll at least be a little better and it has yet to be the case. I’ve done everything any Doctor has ask of me which in turn has only made my medical bills get bigger. I have yet to find help.
The idea of the long car ride makes me cringe. Is it a possibility have the test done hear and then see you? Along with a list of Doctors in the NW do you also have a list of what type of Doctor is the best to see, or even which tests should I have done for best diagnosing and treatment of PN. I know I have already been diagnosed by OHSU, but that was only from a image guided nerve injection which I thought was to diagnose my SI (although my PT has also confirmed my PN).
Thank you for any help you can offer.
Thank you for your compliments.
As for a list of doctors in the northwest…I am sad to say I am unaware of any others.
The gold standard to diagnose PN are image guided pudendal nerve blocks. You might be able to get your PCP to order them performed by a radiologist under CT or MRI guidance.
Other than that, I do see a good number of people from Portland and would be happy to have a look.
Kind Regards, Dr. Attaman
Hello,
I believe I have been dealing with this issue for about 4 years now. Been dealing with ED, difficulty urinating and very little urge to urinate. Lots of tightness in the thighs and buttocks. I am 29 with a girl friend and we have no sex life as I am incapable of getting an erection. I was seening a pelvic floor specialist for about 12 weeks and saw some improvement as she was confident this was a pelvic floor issue. But maybe felt about 60 percent better at best. I have a lot of numbness in the pelvic region and after seeing my main doctor last week, he believes that this is nerve related, especially since I have undergone all the other tests like CT Scan cystoscopy, Penile Dopler Ultrasound, testosterone check, even had an MRI on my lower back last year thinking it was back related.
I am fortunate to be in a good location geographically in terms of finding a person who handles this type of ordeal as I live in Baltimore, so Johns Hopkins is who I have been referred to. Don’t think I can go wrong there. I am seeing one of their urologists this afternoon so I’m hoping I can get steered in the right direction as I have been told by one urologist that this was all in my head. Any other advice would be greatly helpful. I’m hoping I’m on the right track to getting some long awaited answers.
Dear T,
I’m sorry to hear you are suffering like this. I cannot give any specific medical advise unless you are an established patient of mine. I do perform video consultations for patients all over the world. If you are interested, please contact my office. Kind Regards, Dr. Attaman
Hi, I was diagnosed with PN 14yrs ago by Dr. Stanley Antalak in Mn. Went through decompression surgery, years of blocks, was also diagnosed with IC years into PN physical therapy. Had ketamine infusions, unfortunately nothing has helped. Having over a decade of chronic pain turned into pain syndrome and PTSD. I live in Florida now, having to explain my condition, they all have not a clue what PN is. I am fortunate my neurologist in Mn. Has taken over my care after Dr. Antalak retired. I agree, education needs to reach physicians and the general public. I do have a question, does spinal cord stimulator seem to have success with patients like me? Do you think I have Permanent PN damage because of the duration and little success to relieve pain?
Dear LC,
I cannot comment on your specific conditions due to the medicolegal environment in the US. However, yes, in general spinal cord stimulation is worth a try in intractable cases such as this. Kind Regards, Dr. Attaman
Lisa,
Can you please tell me who your neurologist is? I am in MN too and looking for someone who knows about PN.
Thank you!
Michaela
Mykayla, have you found anyone in mn yet? I’m struggling too and can’t find help
Dr. Attaman : Are there any doctors in Maryland area or Southern MD who specialize in treating Pedundal Neuralgia. I’ve tried different pain meds but side effects were very bad and I couldn’t deal with them so stopped. Would accupuncture be a possibility and do you know of the Kyrobak equipment for LBP?
Dear ND,
I am unaware of any. You could search on pudendalhope.org for a physician in the area. Unfortunately, there are very few of us. Kind Regards, Dr. Attaman
Dr. Attaman,
You mentioned that the gold standard to diagnosing Pudendal Neuraligia is image guided Pudendal Nerve Blocks. Are these the types of image guided nerve blocks that are fairly quick for the physician to perform, typically at a surgery center, and require no actual surgery, stitches, or down time for the patient? Are there any risks associated with having an image guided pudendal nerve block done? Also, if the nerve block is done, and there is a relief of symptoms, how long is it before the symptoms come back? Can a man sexually function normally afterwards?
Thank you,
Dan
Hi Dr. Attaman, I am a male 45 that is currently having pain issues in my buttocks and then what seems like a radiating pain down my inner right thigh. I recently started riding a rode bike, biking upwards of 25-40 miles a week. I also have recently started experiencing twitching in both of my calves. The pain in my buttocks and inner thigh is not constant. I notice that it builds over the day depending on my activity. If I am on my feet for long hours or if I go for a moderate hike, jog, or bike ride the pain starts to build and crescendos late in the afternoon. It gives me great anxiety because I have never experienced anything like this in my life. Another can of worms is someone mentioned this could be attributed to an STD. I have always known I have herpes oral and have recently tested positive via an IGG blood test. I took the Western Blot for genital herpes and was negative. I have never had an outbreak and have not had an oral outbreak in over 12 years. Do you think this is related to the pudendal nerve or some other nerve condition? Maybe I should stay off my bike for a few months? I live in Nevada, but I did see there are some specialists in Santa Monica. I thank you for your time.
Dear BB,
It is unfortunately not possible for me to diagnose you unless I see you in person. However, pudendal neuralgia was first recognized in long distance bicyclists! It is a common issue with such folks. Best, Dr. Attaman
I have been reading up on pudendal neuralgia for a while now and have learned that there is a big difference between pudendal neuralgia and pudendal entrapment. I have heard that entrapment is much more severe and causes nerve damage. Does the same go for pudendal neuralgia? I believe I have it because pf the tightening of my pelvic floor irritating the nerve. I think I have pudenal neuralgia. I have had it for about 9 months. If I have it does this mean I have nerve damage? i just need to know if I can solve this with Botox or some other thing that will make my muscles calm down if there will be and remaining damage to my genitals. Thank you!
Dear T,
It is unfortunately not possible to answer your complex questions via this blog. I would suggest you schedule a phone or Skype consultation with me and we can try to figure things out. Kind Regards, Dr. A
Hello Dr Attaman.
My name is Tony . I live in Alberta Canada. I am trying to find answers to my situation. In Dec of 2014 I was diagnosed with a bacterial infection in my prostate. I tried to take cipro but this did nothing. I turned to natural Doctor who was able to help me. The burning feeling I had left within a few weeks of treatment. However i then started to experience a heavy feeling in my testicles. I did not think much of it and ice seemed to help. After a couple of weeks I decided to speak with my doctor md. Who suggested an untrasound. This showed nothing and pain continued. I was provided with pain medication. After a few more visits and nothing to report and a long wait referral was then provided to a local urologist. I decided I needed help. I found that what I may have is pelvic floor spasms. I contacted a pt in town only 1 of about 12 in the province. At first treatments helped. I decided to have sec with wife first time in many months as when I did I had psin that would last several hours. Thus time it lasted 10 days. It took 3 treatments of pt to get me back to what felt normal. Continued with treatments with pt. ni was able to spread them out to 3 weeks. Then another set back again with sex. Once again 10 days. When I have the set backs I can not go to work. Nothing. I am in psin. As a result has been 6 months since sex. However during thst time I have problems going far when driving. I know can barely make it 10 minutes from home and I have psin. Urologist said I have pelvic floor dysfunction. I take flow max and Tylenol. However these are not helping. Ct scan showed nothing. In taking with pt she feels that now nerves are problem more then muscles. Ice nor heat helps. Tried using internal tens machine but that makes it worse. Pain is from tip of penis down shaft into scrotum and below. Sitting is getting harder to do. I feel most lower is comfort on left side. Don’t tines I feel pain. Sometimes pinching. Some times dull ache. As o am writing this I found a couple of T3’s in house. Took that and psin reduced. I have tightness/discomfort/pain. In lower back hips and thighs. I read you can have pn and pelvic spasms. This is from sane hope website you mentioned. O have many symptoms that the web site mentioned. Constipation. Straining. Incomplete urinatikn. Long lasting pain after sex. Etc.
I believe the purdenal nerve is what is causing this. That it was caused due to an infection. That with pn Physio does not provide help ( saw this on another site). That I have more pn symptoms then pelvic syptoms. I just have a gut feeling. If I am wrong I am wrong but I am 43 and until last Dec all was good. Lmk. Thank you in advance.
Ps I am not sure how your reply will come. If there is a way to send to me directly that would be great.
Dear T,
I’m sorry you are suffering. I would suggest you schedule a consultation with me via phone or Skype. Kind Regards, Dr. A
Hi Dr.Attaman
I have been getting treatment in New York City with superficial trigger point injections and pelvic floor physical therapy . I started to see results but one day I woke up and I started having excruciating pain with burning inside the pelvic floor sit bones legs and I am not sure why you got to that point . I know My Mri shows scaring of the PN, for some reason the burning is not subsiding. I was hoping you can lead me on which way to go, I am a little confused about all these injections that they do have out there for PN at Rochester clinic, Dr. Conway New Hampshire or Dr. hibner in Arizona. Or do I just go to a pain management and they do also some kind of trigger point shots which I think is different than the superficial shots IV guided. So my question is If the Mrn shows scaring on the pudendal nerve, and the superficial trigger point injections I get which consist of marcraine/lidocaine and steroid injections, which at times I get relief for three hours at most, what do I do next? Do I do other kinds of shots, this is way to confusing. thank you for all your help
Dear A,
Unfortunately trigger point injections are not useful in diagnosing pudendal neuralgia, if that is what you are concerned about. I would recommend you see somebody close to you like Dr. Conway. You want a physician that is experienced in pelvic pain, as most physicians, including pain doctors such as myself, do not have any interest in or experience in treating pelvic pain. I do see people in consultation from around the world and would be happy to see you via an in-person visit or video conference. Kind Regards, Dr. Attaman
Ji have had tailbone pain for three years. It goes in pain sprouts on and off. Last year had an X-ray that showed a fracture. After that I had trigger point injections that helped. Now in the last month the pain has come back. Would I be a candidate for this treatment you do?
Dear Misty,
I would be happy to see you in consultation to see if this is something I can help you with! Best, Dr. Attaman
I apologize if anyone has asked this question but I was wondering what the difference between pudendal neuralgia and pelvic floor dysfunction is? Does pelvic floor dysfunction still effect the nerve? I know they go hand and hand and hand occasionally but can pelvic floor dysfunction just effect the muscles and not the nerve? Thank you!!
Dear Taylor,
Pudendal neuralgia is irritation of the pudendal nerve. Pelvic floor dysfunction is when the muscles of the pelvic floor do not work well together. They can both affect each other, and they can occur in isolation. Yes, pelvic floor dysfunction can affect only the muscles and not the nerve. In some cases, the nerve is indeed involved.
Kind Regards, Dr. Attaman
Dr Attaman. I need help with perineal pain got three years. The Dr wants to do Botox injections into muscles that she says are too tight. This scares me to death but I cant continue. I do have pelvic organ prolapse which is what I thought was causing the issue but have been told there is not enough prolapse to cause this. I am constipated constantly despite treatments and rarely feel the correct urge to urinate. I just get pain or spasms. I have other issues that need to be addressed and time I’d running out before a trip to Yelliwstone to see my Grandchildren in 1 1/2 years. Please respond
sir,
I suffered from neuralgia pudentale six months ago following an intense sexual relationship. It burned me and I urinated frequently ! m we gave 30 days of ciprofloxacin in the beginning because it m said that c was a chronic prostatitis abacterial at the beginning . I suffered from a lot of side effects of this antibiotic . Is that the pudentale neuralgia can be the beginning of a multiple ?
Merci beaucoup de votre réponse !
Dear J,
This does not sound like pudendal neuralgia, thought I cannot be sure without examining you. I am available to do skype/facetime or phone consults worldwide. Please contact us if you would like to discuss.
Bon Courage, Dr. Attaman
Hello,
I have been suffering from pudendal neuralgia for about 1 yr. Vaginal, low back, and butt pain. I also have genital herpes. I believe the pudendal neuralgia came from constantly using my vibrator on my clitoris for about 1 year. After I used the vibrator for a year, that’s when I had the pain I listed above. I had a pudendal nerve block which relived my pain for about 2 weeks. My question Dr. Attaman is, if I need to get surgery, can I still get the surgery even if I have genital herpes? I do not believe the herpes caused the PN but the vibrator use did. I never had a problem with my herpes until I used the vibrator for about 1 year. Is it also possible if we could FaceTime? I would like to talk to you about this condition and make an appointment at your office.
Dear Julia,
Sorry to hear about this. I cannot diagnose you without seeing you in consultation. In general terms, I do not expect the herpes to cause this issue. The excellent response to the pudendal nerve block plus the mechanism of injury points toward pudendal nerve issues as the problem. Genital herpes should not interfere with the surgery. I do Skype and FaceTime consults frequently for patients around the world, please contact my office to set one up. Kind Regards, Dr. Attaman
Dear Jason,
I have been suffering with pudendal neuralgia for 5 years. Mine was a result of a laparoscopy gone wrong while the surgeon was looking for endometriosis. I had been seeing Dr. Stanley Antolak in Edina, MN who specialized in PN; he retired, but have since moved to Hammond, LA. I am in pain management, but they know nothing about PN, and I don’t feel they actually believe me when I mention it. I’m suffering. My medication does is too low, so my pain is escalating and interfering with my life. I have been trying to research and find a specialist, but I’m having a hard time. Is there anyone that you could recommend or know of that’s around my area that specializes in PN? My depression from this is starting to take over my life again.
Dear HH,
I am unfortunately not aware of anybody in your area that treats pudendal neuralgia. I am sorry you are suffering. Kind Regards, Dr. Attaman
Do you know of any doctor who practices Alcock canal infiltration with corticosteroids in Texas?
I’m sorry but I do not. Kind Regards, Dr. Attaman
Hi,
I’d be glad to come to see you. My PN is causing a high level of pain all the wai up my right, through my clitorioal, and around my back. My sensitivity test is correct, I can’t raise my leg. I get PT but it’s not helping. I’m waiting for a call for a black from Strong Menorial. Thank you, D.C.
Dear D.C.,
Thank you for your comment. I look forward to seeing you. Kind Regards, Dr. Attaman
pudental nerve can be damaged by laser depilatory procedure?
Dear Maria,
I doubt that is possible. Kind Regards, Dr. Attaman
Hi Dr. Attaman
I have been suffering from pain in my hip and buttock area for a few months now. I have had 2 pudendal nerve blocks which have helped a lot but I still have pain sometimes. Before the nerve blocks, I had internal vaginal pain which is now gone. I also have pain in my piriformis muscle that hurts when I sit and I have pain when that muscle is pushed on. What I was wondering is can pudenal nerve damage cause pain the the piriformis muscle and hip? I have pain when I sit and pain the the piriformis muscle when sitting down as well. Can the pudendal nerve be trapped on the piriformis or hip muscle causing pain??
Dear Ellen,
I’m glad to hear you have gotten relief! That is wonderful. I understand you feel your piriformis muscle is bothering you, but I am willing to bet that its really your obturator internus muscle that is painful, not the piriformis. The obturator internus muscle is most often involved in cases of pudendal neuralgia, indeed the fascia (the outer covering) of the obturator internus helps to form alcock’s canal, through which the pudendal nerve passes. I believe the pudendal nerve and obturator internus are intimately involved and more often than not, both need to be treated. If pelvic floor PT does not help with this muscle, then botox injections often do the trick. I have performed botox injections to the obturator internus on many people. If you get it done, be absolutely sure it is done with image guidance (ultrasound, CT, MRI), as the muscle is very deep and impossible to accurately inject otherwise.
Kind Regards, Dr. Attaman
Dear Jason,
Hello… Do you know if PN can cause aches and pain in the buttock area such as the piriformis muscle? I go to therapy wice a week where they massage that muscle and it keeps going right back to being in pain a few hours later. Also, I’m not too far from your office and I’d like to make an appointment. What is your contact information? Thanks very much!
Dear Valerie,
Yes indeed, this is very common. However, more often than not the obturator internus muscle is involved, not the piriformis. It is difficult to know the difference between these two muscles for most medical professionals, as generally we completely ignore the obturator internus. My contact information is on my website, I would be happy to see you. I see patients from around the world with this condition. Kind Regards, Dr. Attaman
Good Morning,
My daughter believes she has PNE. She is having intense pain running down her leg and on her butt cheek. She said the pain in her butt feels like something is squeezing her muscles in the butt. She has just recently told me she has genital herpes. Can herpes cause PNE? Since she has herpes can she have success treatment from PNE? She has also had a nerve block that did relieve pain for about 2-3 weeks. Thanks.
Dear Karen,
Yes, herpes can cause pudendal nerve pain, but not entrapment per se. It is fairly rare. Yes, successful treatment is indeed possible for this issue. That she had excellent relief from a pudendal nerve block is very promising. I would be happy to see her in consultation. Kind Regards, Dr. Attaman
So if you have recurrent herpes would it cause damage to the nerve or some lasting irritation ? I have been under a ton of stress this year and have gotten a herpes sore almost every month. Usually I get burning pain in the vagina , butt cheeks and down legs and it seems to improve when the sore appears. This time I felt like I was getting one and a sore never appeared but I have not vulva , inside buttocks burning pain ? Could the herpes cause this kind of prudential pain without a sore that lasts. I do have fibromylaiga and myo facial l pain issues and my nerve and muscles are easily irritated but I am not sure if it has now caused a lasting issue since tis been irritated so much this year? IS it possible to happen?
Dear Dr. Attaman,
I have been suffering from perineum pain for two months, as well as sensitivity on the skin on my upper inner thighs and perineum. All underwear causes discomfort when touching my skin. Also, I always have the feeling of skin rubbing against skin if walking without underwear. When I sit, the pain in the perineum increases. After several visits to a dermatologist, several doses of antibiotics, steroid creams, CT scan, predninesone , nothing seems to calm the pain or decrease the skin sensitivity. Last dermatologist i visited is considering a referral to a neurologist. Can Pudendal Neuralgia besides causing pain in the area, also make the skin really sensitive to touch?
Dear K,
This sounds very consistent with Pudendal Neuralgia. Did you read my blog post, and does it seem to match your symptoms? I cannot diagnose you unless you are my patient. I see people from around the world for this condition. I’d be happy to see you in consultation.
Kind Regards, Dr. Attaman
Good morning Dr. Attaman,
Hi… My name is Rachel and I have been getting pudendal nerve blocks which have really helped with my pudendal nerve pain. I would have pain on the inside wall of my vagina. Just recently I was diagnosed with a yeast infection. I did take the medicine prescribed to me but I still have an itch on my mons pubis. I was wondering if pudendal neuralgia can cause the mons pubis area to itch. I do shave that area, but I’ve never had an itch for days after shaving. Like I said, I did get diagnosed with a yeast infection so I was wondering if this itching could be from the yeast or from the pudendal nerve. Thank you very much. Have a great weekend.
Dear R,
Pudendal neuralgia can cause itching symptoms, but it is rare. I cannot give you specific medical advice unless you are my patient. Kind Regards, Dr. Attaman
Hi Dr. Attman, I fell and fractured my sacrum at S3/4 2 years ago. After I lost feeling in my legs, was unable to walk and was unable to have a BM. However, I have no pain. After having my sacrum manipulated, I gained the use of my legs back, but still unable to have a BM. I have been thoroughly checked by colorecatl doctors and now am told that I have Pundendal issues related to my fractured/dislocated sacrum. I see that you treat pain but do you look at all Pudendal issues or just pain? Thanks.
Dear EW,
There is no medical explaination that manipulating your sacrum could restore feeling and strength in your legs, but I am glad they work again. I cannot tell if you have any pudendal issues from the information you have given. I’d be happy to see you in consultation to try to figure this out. Kind Regards, Dr. Attaman
I had emergency abdominal surgery due to an impact to the stomach on May13. My greater omentum was removed and an artery sealed. I had a contusion on the large intestine.
I healed normally , I had severe constipation for several days and strained to have a Bowell movement.
Afterwards I resumed my activities with little pain.
Around the first of june I had a sudden onset of testicle pain. I went to the emergency room on june 3rd and had a sonogram, they found a hydrocelle and a varicocel.
They proscribed Oxicontin for pain.
i was in bed for a week with severe scrotal pain.
I had had a varicocele embolised about 5 years erlier by the South Florida Vascular center. The pain was similar and I assumed it was a vascur issue.
I went to Dr. Siut, a urologist in Stuart, florida for an exam the following thursday. He attempted a prostate exam but my anus was too tight. He scheduled a a transrectal sonogram of the prostate the following morning.
He proscribed tramadrol 50 mg and ciprofloxin
After the attempted prostate exam I felt immediately better. By the afternoon I was driving and functioning. In the morning I had the transcrectal sonogram. The technician almost could not get the probe in.
The technician and the doctor kept focusing on a urolift procedure I had on my porstate in april 2014 byn Dr,. Peritoi of Miami.
First they thought it was cancer, then infection and then a cyst.
That Friday after the two episodes of anal probing I felt immediately better. I assumed it was the antibiotic clearing up an infection that was not detected in any of the urine tests.
Around a week later the pain resumed at a much lower level. I had a consistent testicle pain that started to settle onto my left testicle, I went to the South Florida vascular center. The pain was nearly identical with the pain I had experienced with the varicocele.
They ordered a cat scan with contrast of the veins. They found nothing they could treat.
The cat scans before my surgery indicated diverticuosis. I went to a General Practitioner at urgent care and she proscribed a clear liquid diet for 48 hours and a cat scan with barium contrast.
In the mean time my pain started moving away from just my testicles to my inner thighs and buttocks. I occasionally have pain and discomfort inside my groin above the testicles. I have a few shooting pains down my leg. The most common pain is a toothache like pain centered around my left testicle.
I got a therawand and tried massaging my pelvic floor. No real results
The worse thing I can do is sit. bending causes pain as well. Two or three days of the week I am nearly symptom free. Lying down with my legs elevated gives the most relief. I use pain pills about three days a week
My symptoms seem consistent with pedundal entrapment or injury. I have not been able to get any of the local specialists to respond. I did see someone advertising deep laser therapy for this. Any ideas
Thanks for taking the time to build this blog. It has been very informative
Dear G,
Your symptoms sound very complex. There may indeed be some pudendal nerve involvement, but I cannot tell for sure without doing a complete history and physical exam on you. I’d be happy to see you in consultation. I also perform Skype/Facetime consultations for out of state patients. Kind Regards, Dr. Attaman
Hi, my name is Stephanie. I have suffered all my life from severe menstrual pain. Over the last 6 yrs my chronic pelvic pain has gotten much worse. My doctors diagnosed me with PCOS, chronic pelvic pain, vaginal muscle spasims, ect. I recently had a hysterectomy in June 2016. My doctors swore that this would make the pain stop. It did not. I have had trigger point injectionso in the vaginal canal, been on a plethora of medications, and have seen over 18 different specialists/doctors. I have painful intercourse and if I have an orgasim, I’m in sEverett pain for 30 mins to 3 hrs after. This happens whether it is intercourse induce orgasim or clitorial induced. I also have pelvic pain all the time (worse with intercourse/masterbation/orgasim). Although I no longer have my uterus or my cervix, I feel like I am having severe cramps, pressure, and tightening all of the time. Could any of the above information about PN be my issue? If it’s a possibility is there a known doctor in the San Diego, CA area? If not, the closest doctor? I am willing to travel. I really just want to have my life back. This is mentally and physically taxing. Please help!!! Thank you
Dear SS,
I’m sorry to hear you are suffering. This sounds like a complex case. There may be a component of pudendal neuralgia to this though I cannot be sure without evaluating all your records and doing a history and physical with you. Kind Regards, Dr. Attaman
Hi do you deal with non relaxing puborectalis/levitor ani as related to pudendal nerve damage secondary to traumatic sacral nerve fracture without pain? If so, I will schedule an appointment.
Dear JR,
This is a complicated matter and I suggest a clinic consultation to discuss. Kind Regards, Dr. Attaman
Hey Doctor Attman,
I was wondering if PN can cause a tingling/burning sensation in the area where the pubic hair grows? I have a pudendal nerve blocks in the past which have helped so I think I do have PN. But now, I have a constant tingling and burning in the pubic mons. Could this be from the pudendal nerve damage?
From,
Briana
Dear B,
Yes absolutely the pudendal nerve does provide sensation (and pain) to the region you describe (the mons pubis region). I’m glad you have found a diagnosis and hope this resolves for you. Best, Dr. Attaman
Dr attaman….I have heard recently about pudendal cryoablation…can you give me any information on that? Do you perform that procedure
Hi Dr. Attaman, Try and make this short…. started with a left side burning in my labia minora 6 weeks ago with sharp pains in lower back and hip. Now have burning, which moves around from rectum, both labias and ureter/clitoris. driving me mad!! Sometimes it just disappears for two or three days. Burning is gone when I wake up in morning only to start up again. worse when doing alot of bending. Any Professional Ideas??? Thank you for your time! Karen
Dear KO,
This sounds as if it may be pudendal nerve pain. Treating this is pretty complicated. I’d be happy to see you in consultation and go from there. Best, Dr. Attaman
Hi there !
Just some comments. It appears I have PN related to a left hip surgery to debride a labral tear 7/7/15. Symptoms started 6 weeks post-op. So it has been over 1 year for me now. Took me a long while before I found a gyno MD who said YES this is related to your hip surgery. One gyno MD diagnosed me with vulvodynia, to which I was still not satisfied as I had a obvious catalyst to the change in my body- SURGERY. In addition, I have pelvic floor dysfunction. So I have been in PT for that…and my PF muscles have improved. We just did my first nerve block less than 2 weeks ago. I can say there is SOME relief, but it is still there…. so we will try again with a 2nd injection. IF needed we will try botox into the pelvic floor muscles. Boggles my mind that muscles and or nerves can make one feel like they have a yeast infection.
It has been a long long long road……it has taken a TEAM of psychologists, massage therapist with reiki, guided meditations, my awesome gyno MD Dr. Kurt Christopher (S FL, he was in NY), ortho MDs ( who seem to refute this is related to the hip surgery and who have really been of NO help).
Overall, I found gyno MD”s and ortho MD’s lack knowledge in this area. To which I went through some serous mental anguish. So I thank you for your work in this area. Please help educated the medical community.
I do have hope. I am hoping that I can be fully cured. In relation to others, I have learned that I am more of a mild case, BUT it still does not take away from my experience of hell. But I am grateful, that hopefully due to my relatively mild case, that I can be fully cured.
Oh and also I have fully come to believe in SOUND therapy for the nervous system. Healing meditation music, gongs, crystal bowls, etc. I go to live events and use an app Insight Timer and youtube for videos. Kudalini yoga mantra are also soothing. So FYI for anyone. Also helps with the stress and anxiety of it all.
Needless to say….i hate to have regrets…but that surgery was not a good choice….but I made an “informed” decision at the time. Turned out to be not the best decision of my life.
Healing vibes to all!
Stacy
Dear Stacey S,
Thank you for sharing your journey. It is indeed sad that the medical profession is so ill aware of pudendal neuralgia. It sounds like you are on the healing path, thank you for giving hope to others suffering from this! Merry Christmas, Dr. Attaman
Hello dr.
Can pudendal nerve damage be caused by rough unprotected oral sex? (Use of teeth). I noticed incredibly red meatus afterwards, with pain/burning/sensation.
Initially I had NGU symptoms(infection)which cleared after standard CDC treatment for 2+months. Pain in the urethra persists for 3+months now. A constant urethral pain 24/7. 2nd urologist seemed confident it was CPPS, saying “it was all in my head”, but I think otherwise.
I beg for your prompt reply.
Dear DET,
It is certainly possible, though I cannot recall another patient with this cause. Urethral pain is not typical of pudendal neralgia, though penis pain is. I’d be happy to see you in consultation. Best, Dr. Attaman
Pudendal nerve trauma due to rough oral sex. Ever had a case?
Dear DET,
It is certainly possible, though I cannot recall another patient with this cause. I’d be happy to see you in consultation. Best, Dr. Attaman
I was diagnosed with pudendal neuralgia this summer and have shown little sign of improvement. I can’t afford physical therapy until october when my insurance covers it again. This condition has effectively reduced me to a eunuch: i can get an erection, but all sexual stimulation brings me is pain, and the nerves in the crotch give me pain whenever i sit or lie down. My urologist recommended PT and is just having me take it easy, but has no real plans for treatment he can offer.
I’m 35, male, and never had a girlfriend. This happened right around the time I was finally getting the courage to try to talk to women again, because it’s been really getting to me, and I’m afraid to wake up tomorrow and be 50 and alone. Since coming down with this condition I’ve felt completely helpless and hopeless: I have no idea if I’ll ever get better, and even if I do, I’m afraid it will be just in time for my reproductive abilities to shut down on their own due to age. I’ve been an emotional wreck for months and I don’t know who to turn to.
I’m also in Arizona, but there appears to only be one clinic that treats this condition, and it might be just for women. I’m not sure.
Dear M,
I’m sorry to hear that. There are unfortunately not enough treatment centers for folks suffering from this particular condition. Merry Christmas, Dr. Attaman
Dear M,
I’m very sorry to hear your story. I hope you are doing better by now. If not, I’d be happy to see you in consultation. It sounds like there are many treatment options that have not be yet explored for you. PT can certainly help, but is only one of many treatment options. Usually I employ multiple treatment options simultaneously for best outcomes. Best, Dr. Attaman
Hi Dr. Attaman, I’ve had penis pain at the tip, increased pain while sitting, pain after sex and pain around the pubic area for 9 months. It came on suddenly day after having sex in March . And my symptoms always worsen though out my day. The only relief i get is from klonopin when the pain hits full throttle. My main triggers are sitting and driving. I’ve been diagnosed with nonbacterial prostatitis, IC, pelvic floor disfunction IBS and sibo all within this last year. Does this sound like a possible pudendal neuralgia issue? I live in Portland, OR. Thank you …Tim
Also, my 2 cystoscopy’s came back normal and urodynamics was normal.. Thank You- Tim
Dear Tim,
It is certainly possible it could be pudendal neuralgia. Why don’t you come up to Seattle for a consultation? I’d be happy to check this out. Kind Regards, Dr. Attaman
Hi Doctor Attaman,
I have been dealing with PN for quite a while now. I have been getting pudendal nerve blocks which have truly helped my situation. Almost to the point where my pain was completely gone. Just recently, I had intercourse with my husband and 2 days later I had a frequent urge to urinate and bladder pain. I went to urgent care and they found bacteria in my urine. When the urinalysis came back, it was negative. However, they did give me Bactrim and prescription azo to the with the pain. Now, I feel like I’m back to square one when I first got PN. My bladder feels like it is on fire on the side where I have PN. This started after I was told I had bacteria in my urine. My question to you is, can PN cause you to feel like your bladder is hurting/burning? Could the bacteria in my urine have caused the PN to re activate itself?
-Bri
Dear Bri,
I’m sorry to hear of this. The pudendal nerve can cause some uncomfortable bladder sensations, but rarely is it the primary cause of bladder symptoms. Kind Regards, Dr. Attaman
Hello Dr. Attaman,
My name is Deb. I’ve been suffering with pundendal neuralgia for 16 years now since I was 28. I’m now 44. I was always misdiagnosed with vulvodynia and in 2014 I made the biggest mistake of my life after being misdiagnosed again and having a vulva vestibulectomy. Let’s just say that the life I thought was bad became unbearable at that point to where now I’m basically home bound and lost so much in life. Well I’ve been through it all. I need advice right now. You see I’ve had almost everything done from blocks to pulsed radio frequency, to ganglion impar blocks, to electrical spinal stimulater, a partial hysterectomy and now facing the choice of cryoablation or surgery. I’ve also tried every medication and also years of physical therapy to no avail. So, I’m so afraid of both procedures but I can’t live like this anymore. The pundendal neuralgia isn’t just the pain anymore it has also effected my bowl and bladder now and it’s very difficult to walk along with all the other signs and symptoms that go along with this monster. Please can you shed some light on my situation. Thank you Deb
Dear Deb,
I’m sorry you are suffering. This case is too complex to address over the internet. I’d suggest a consultation in clinic to try to figure out next steps for you. Best Regards, Dr. Attaman
Dr. Attaman,
I have been diagnosed with PN and suffer on a daily basis. It’s a terrible condition and I know how everyone feels who has asked all of this questions. It’s living with a monster. Anyone I was wondering if you could tell me what you know about cryoablation and if you know of any doctors besides Atlanta Georgia that does this procedure. Thank you so much. Feeling hopeless Sophie ????
Dear Sophia,
I’m sorry you are suffering. Cryoablation involves freezing a nerve with an iceball generated at tip of a thick needle. The nerve stops functioning for 2-5 months, then regenerates in most cases. If cryoablation is properly performed, the area in which the nerve goes will be numb. Because of this numbness, we try not to perform cyroablation on the pudendal nerve as this would render your genitals numb. Kind Regards, Dr. Attaman
Dr. Attaman,
How do I schedule a consult with you?
Dear J.H,
There are multiple phone numbers and email contacts on my website. Please have a look.
https://jasonattaman.com/contact/
Dr. Attaman
Hi Doc,
2 weeks ago I rode my push bike some 450 miles over two days. Spending about 15 hours in the saddle on both days. About 2 days after a slow insidious onset of a unilateral (left) dull ache and also occasional sharp shooting pain, hypersensitive (burning feeling) to touch developed to the point of 10 out of 10 pain which remained constant for the next 5-6 days. Doctors largely unsure of cause as physically appeared normal and everything appeared within normal limits. Ended up in the ER and not much was done. In the last say 2-3 days the pain has fortunately subsided substantially to about a 4 out of 10 and I am much less reliant on analgesics. The pain is still constant. I suspect given the symptoms and history I have developed a case of PN. I am extremely concerned as I am only 23 years old and cycling is a massive part of my life. Given the pain has subsided in the last couple of days is it possible that this will self resolve entirely? Is this something I am going to experience my whole life without treatment? Or could my Dx be wrong or is the pudendal nerve beyond self repair?
Keen to know your thoughts as finding somebody with knowledge and or experience in treating Pxs with this nerve is difficult.
Kind regards,
KT
You do not describe where you pain is, but I am assuming in your pelvis and or genitals? I cannot diagnose you over the internet, but the pudendal nerves do indeed course through this region. I’d be happy to see you in consultation to figure this out. Kind Regards, Dr. Attaman
Hi doctor I had all the symptoms of PN I am thinking in surgery in nantes France but I want to be absolutely sure with the right diagnosis because here in Mexico is very uncommon this problem
I have dealt with this issue too. It started 3 years ago when my immune system and allergies took a steep deep due to stress and inflammations. I would say I rarely get it anymore. A friend of mine recommended the use of PeaPlex. I ordered it from RS4supplements.com and it helped me a lot.
Hello, Can different procedures outlined you be performed during pregnancy?
Dear Dr. Attaman,
Do you ever come across men who are experience Post Vasectomy Pain Syndrome that involves damage to the pudendal nerve?
My husband had a vasectomy 4 years ago, a reversal three years ago, and operates on a daily pain scale reading of 5-6, with frequent spikes that hit close to 8. We’ve tried Scrambler Therapy® Technology (such as that done by Dr. Edmucd Boese in Eagle, Idaho), medication, pelvic floor therapy, anti-depressants, gabapentin, cannabis in three forms, to name a few. The RF ablation treatment came up via a participant in a forum I belong to for PVPS, and I hadn’t heard of it. I am curious if you have seen post-vasectomy pain patients who an tie their pain to this particular nerve, and if so, if you’ve seen success in treating the pudendal nerve.
Thanks so much!
Jenn Braden
Dr Attaman,
I have a history of IC and PFD but both very well managed and other than the occasional bladder flare or mild pelvic floor tightness, I’ve been 100% pain free. I’ve had pudendal nerve irritation for only one week. It started after my pelvic PT worked a bit too aggressively on obturator. Now I cannot sit without pain. It is mostly in my perinium but sometimes moves forward to the left wall of my vagina with an aching ticklish feeling and altered sensations. My PT said the muscles on my left side are in complete shortened spasm. She got one to release, piriformis I think. Is there a good chance that if she can get obturator and the other remaining muscle to calm down that the nerve irritation will go away? This has ruined me, all I can do now is lay on the floor and cry. I’m terrified to try any other treatment, even my pelvic PT stretches, in fear of making the pain worse or permanent.
Though you should still have some fairly powerful days, correct
administration of depression will make things much easier for
you.
Dr. Attaman,
I have been dealing with PN for 2 years now. I’ve been taking the suppositories and oral valium/baclofen. They help but never completely alleviate the pain. I seem to be getting better over time just VERY slowly. I’m really into weightlifting and exercise. In your experience, does lifting weights make PN worse or slow down the healing process?
Thanks in advance!
John
I had pelvic mesh implanted for POP in 2014. Dr Veronikas removed all the mesh in November this year. All good now except the exact pain you described as PN. Only on left side. Subsided in labia. Settled into small spot on left hip and anus. Sitting is uncomfortable. There is a Dr. listed on the website you mentioned- office in Franklin, Tennessee. Do you know of someone there? I live in Hendersonville, Tennessee. Dr Veronikas was located in St Louis. So, I have traveled for care, not multiple trips.
Thank you!!
Hello Dr. Attaman
My name is Anna
For the last 7 months I’m having this burning pain near my urethra canal, plus vibrations, tingling and pin and needle sensations. Sometimes there is this buzzing feeling in my left leg as well. I had all the necessary tests done at my urologist office, no infections has been found.
Do you think it’s possible that I may have PN base on the symptoms I described ? My urologist suggested gabapentin for nerve pain.
Could you also recommend a good specialist in Pudendal Neuralgia, in New York City or Long Island ( New York )
I would really appreciate your help.
Thank you very much, I’m sorry for my English.
Best regards
Anna
I have pedendal nerve pain for many years, but also developed bad sciatica down into my feet, after years of suffering and havinig atrophied muscles. I decided to get back surgery, it did not help my sciatica my pudendal;nerve issue was not real bad at the moment but was coming back some after i got it calmed down for 6 years. After starting
physical therapy started irratateing the nerves thou the therapy was simple, i avoided exercise years back because of pudendal nerve pain. Only did therapy for a month they sent me home and i did home therapy till i get stronger then they would have me come back for more aggressive therapy i never went back. Also i quit all therapy started to having to much back of leg issues. I did a exercise on my own where you sit in chair and do air cycling i only did it once and a hour later my pain in the anus first perinium and penis started back like 6 rears ago burning ect. But also it seems my sciatica got worse it grows worsre with sitting with the other problems to and better whe i stand . My sciatica will still hurt some when walking. Have you ever treated someone who had both coming fro the buttocks. Im wondering if i had developed pirisformas syndrome, where the pudendal nerve sciatica are entraped in same area. thanks for reading Bill from michigan
Hi I am in living in New York City and I am trying to find a good specialst like yourself for PN. Do you know of anyone?
Thanks
Justin
i’ve been seeing a pelvic physical therapist for 3 months now, and i’m starting to assume that i have a pinched pudendal nerve or blood vessel in the alcock’s canal near the obturator internus. is there any specialist you can recommend in the atlanta, georgia area? i’ve been dealing with this for about 9 months after a cystoscopy and a retrograde urethrogram a urologist did, and another urologist said that those procedures caused hypertonic pelvic floor dysfunction and i’ve been in pain ever since.
Dr Attaman
Can anti depressants cause problems with the Pudendal nerve ? I felt massive cramps in the perineum while I was on ADs and I’m left with a constant pain and a bunch of other related symptoms that just don’t go. It’s been 5 years and the pain just doesn’t go.
I have been suffering with pain (which usually manifests as a raw and extremely itchy feeling) for almost 2 years post my 2nd C-section. Confirmed pudendal nerve is thickened on my left side (at alcocks canal) via MRI and have received 2 PN blocks (which helped immensely). The intensity and frequency of pain definitely got better after years of pelvic therapy and nerve blocks. Is there anything else you’d recommend I ask to try? I’m so frustrated that the itching is back (rectal pain and itching). Was hoping the nerve blocks would solve the issue.