If you suffer from intercostobrachial neuralgia – a kind of armpit nerve pain – Dr. Jason Attaman can help. Located in Bellevue, WA, Dr. Attaman treats patients throughout the Seattle area, sees patients who fly in for treatment, and provides telemed appointments where appropriate. You can call us at 425-247-3359, email us, schedule an appointment with Dr. Attaman online, or you can read on to learn more about intercostobrachial neuralgia and possible treatment.
What is intercostobrachial neuralgia?
Intercostobrachial neuralgia is a rare but very bothersome nerve pain issue, in which nerves nerves running through the upper thoracic spine, armpit, upper inner arm, and upper chest wall are damaged and cause pain.
Who gets intercostobrachial neuralgia?
Most patients suffering from intercostobrachial neuralgia are women who have had mastectomies, typically following breast cancer surgery. Sometimes referred to as chest well pain, this condition typically arises because the surgery disrupted nerves in and around the armpit. This is known as post mastectomy pain. Armpit nerve pain also can develop after radiation therapy to the lungs and upper chest wall. Trauma to the ribs such as rib fractures can cause intercostobrachial neuralgia. People who have had thoracotomy surgery also develop it. This is known as postthoracotomy pain. For that reason, intercostobrachial neuralgia may also affect women who had breast augmentation or breast reduction surgery.
Men also can suffer from intercostobrachial neuralgia, though it is much rarer in men. I have had a handful of men present to me with this problem, so intercostobrachial neuralgia is not exclusive to women by any means.
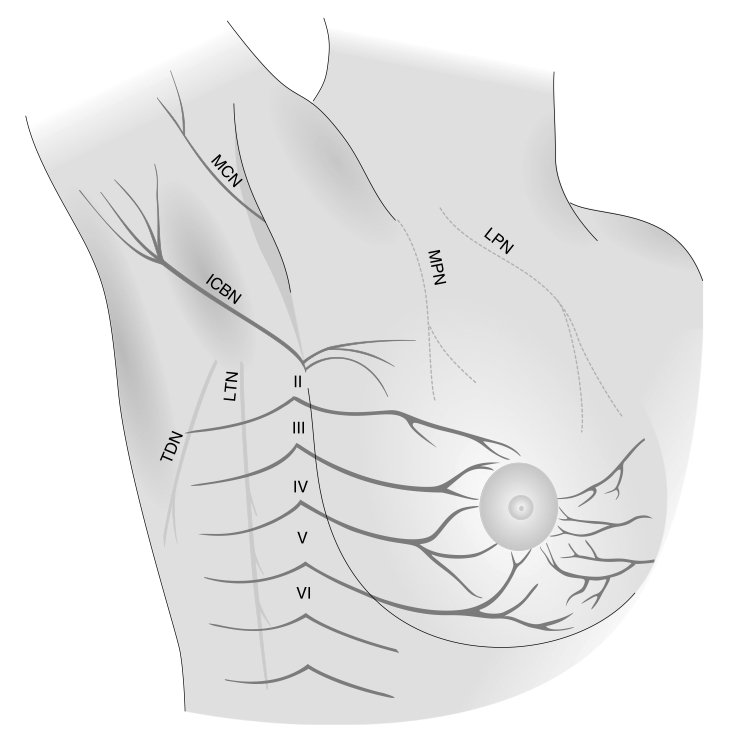
Intercostobrachial Nerve (labeled ICBN)
Intercostobrachial neuralgia occurs in 25-60% of patients surviving breast cancer surgery, but is often overlooked
The unfortunate aspect of intercostobrachial neuralgia is that very few physicians are aware of it, and the pain it can cause. Thousands of people suffer annually from this pain after getting surgery or radiation therapy and their surgeons never tell them what is causing the pain. Frankly, I suspect many of the surgeons do not know that this can cause a serious pain issue. Secondly, most surgeons do not enjoy dealing with chronic post operative pain, in particular neuropathic (nerve damage) pain. Neuropathic pain is difficult to treat appropriately, but the first important step is a proper diagnosis.
How is intercostobrachial neuralgia treated – and the nerve pain brought under control?
Especially, if I see a patient with a history of the above-mentioned medical issues, I will see if their pain fits the anatomic distribution of the intercostobrachial nerve. I test the function of the nerve by testing sharp sensation, testing vibration sensation, testing cold sensation, and testing light touch. If I find these sensations impaired or painful, my suspicion of intercostobrachial neuralgia is raised.
Next, I generally suggest a diagnostic and (we hope) therapeutic block of the intercostobrachial nerves using a strong local anesthetic and steroid medication. Typically I will use x-ray or ultrasound guidance to see the 1st through 3rd thoracic nerves as they pass between the ribs. These three nerves collectively form the intercostobrachial nerve. I will then inject some strong numbing medicine and some anti-inflammatory medication onto these nerves. This is called an intercostal nerve block.
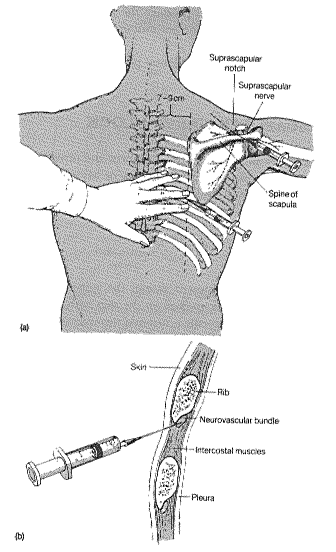
Intercostal Nerve Block
If when I inject this medication mixture onto the nerves the patient’s pain goes away and they become completely numb to sensory testing in the typically painful area, I can confirm the diagnosis of intercostobrachial neuralgia. The numbing medicine typically lasts 4-12 hours during which time the patient is usually very happy as this is often the first and only pain relief they have ever had for this issue.
Next, the numbing medicine wears off and the pain may return. We then wait a few days for the anti-inflammatory medication to take effect and produce longer term pain relief. I have had a handful of patients get 100% complete resolution of intercostobrachial neralgia after these injections. Many, however, get a few months of relief and then the procedure can be repeated as needed if the pain returns.
If I find that my patient gets excellent short term but poor long term relief from the intercostobrachial nerve block, we can consider a procedure called pulsed radiofrequency treatment of the nerve. You may read about it on wikipedia here. This treatment uses radiofrequency energy to deliver electromagnetic pulses to the injured nerves. It is safe and non-destructive. Through mechanisms we do not understand fully, this procedure can help restore normal function of the nerves. This is called neuromodulation in general terms.
If the above does not work, we can consider a pain-reducing device called a spinal cord stimulator (SCS). This device is like a pacemaker for pain. A thin wire is placed alongside the spinal cord where the nerves forming the intercostobrachial nerve emerge from the spine, and a small electrical current is used to block the pain signals from reaching the brain. This is a surprisingly very safe device that is used for many types of intractable nerve pains, not just intercostobrachial neuralgia.
There are also medication options that help reduce nerve pain that can be used as well. Unfortunately, by the time most patients with intercostobrachial neuralgia see me, they have tried various medications.
Does physical therapy help with intercostobrachial neuralgia and armpit nerve pain?
Physical therapy is, unfortunately, generally ineffective for intercostobrachial neuralgia given the nerve is usually too damaged. Sometimes the nerve may be irritated by tight muscles or scar tissue, which physical therapy can address. If I think that PT will help, I always like to get it on board with my patient.
What now?
In summary: if you have had chest wall or breast surgery or chest wall radiation therapy and are suffering from burning, tingling pain coming from your upper thoracic spine, going into your armpit, upper inner arm, and upper chest wall, you may be experiencing intercostobrachial neuralgia. The good news is that there are treatment options available. If you suffer from intercostobrachial neuralgia (or think you might), feel free to call my office at 206-395-4422 (Seattle) or 425-247-3359 (Bellevue), or to schedule an appointment online.

I found your web page very informative.
I had a bilateral mastectomy with chemotherapy, radiation, and finally reconstruction. Oncologist tried Gabapentin with no success. I tried acupuncture with no success. Physical Therapy has helped some with the tightness across chest, cording, and lack of range of motion of shoulders.
It has been almost 3 years. Most of the areas around and in between the scars are numb. However, sometimes the chest is so over sensitive that I can’t stand to wear clothes sometimes. The constriction pain can be so tight around the chest and left arm with stress that you feel like you are wrestling with a boa constrictor. Unexpectedly, you will jump from nerves that feel like biting ants. In addition to the tightness and the bungee cord feeling and ants, there is also the duct tape feeling and now a burning sensation. The burning sensation is on the sternum and under the left breast. Like the ants, it comes and go. Then there is the phantom stabbing nipple pain and pain that I felt in the left breast before the cancer diagnose in the right breast. I have difficulty squeezing a lemon, grating food, or the hand over hand action. Pushing overhead, I am still real weak. Lately, I started having muscle spasms in the right pectoral muscle especially during hand cross over body. If I do not exercise, it gets tight and stiff still. Scars on the chest sometimes feel and look like adhesions. They still pull a little with certain activities and exercises.
I am at a point where I wish to address the nerve pain again but don’t even know who I should schedule an appointment with in Oklahoma. What specialty? Do you have any suggestions?
Dear RL,
Thank you for your kind comments.
The type of specialist you need is an Interventional Pain Management specialist. I do not know anybody specifically in Oklahoma. If you cannot find anybody locally, we routinely host interstate and international patients here at my clinic in Seattle. If you would like to schedule a consultation and possible treatment, I am happy to see you.
Unfortunately, there are very very few physicians worldwide that treat intercostobrachial neuralgia, or even understand that the condition exists…
Kind Regards, Dr. Attaman
This sounds like what is happening to me.
I recently fractured a rib, and since then I have been experiencing pain under my arm and it runs into the side of my breast. It is very painful when I lay down, turn over begin to sit up and I tell my husband that it feels like a burning charlie horse or severe cramp. I have been wondering if I should get a mammogram but because of the rib fracture that is out. Should I get seen by a doctor for this matter?
Hello LH,
This could be intercostal neuralgia, or inflammation of the intercostal nerves. You should certainly seek the opinion of your PCP, but a mammogram has nothign to do with rib fractures or rib fracture pain. You should read my blog on intercostal nerve pain here: https://jasonattaman.com/intercostal-block-shingles-pain/
Best, Dr. Attaman
I have never had surgery of any kind but have had this pain in my left breast for years. The pain has been increasing to the point that I am often unable to leave the house. Doctors are unable to diagnose me, much less treat me. I am a 62 year old woman.
I have been diagnosed with small fiber neuropathy in my feet and legs. That was 6 years ago but a few months ago I started getting pulsing burning in my right breast and under upper arm. I’ve had 2 Drs manually check me for lumps and lymph nodes. Normal. I had a mammogram. Normal. The pain will be bad for periods of time and then ok. I have not had any surgeries in this area. I do have an appt. with my Neurologist and getting another opinion with a surgeon who specializes in breasts..not that I’m getting surgery.
Does this sound like the nerves you are describing here?
I cannot diagnose you over the internet, but the intercostobrachial nerve certainly does course though the area you describe. Best of Luck, Dr. Attaman
I had pain in my neck, right shoulder, upper back, and right arm. There was coldness in my arm and numbness in my pinky and ring finger. At times, I would have burning and swelling under my arm and pain that, at times radiated to the ribs on my right side. I finally had cervical laser spine surgery because there was a bulging disc at the C6-C7 level and they also lasered some arthritis in the other discs.
My arm is so much better, but I still have the burning and swelling in my armpit. It has only been 2 wks since my surgery; do you think this problem will go away in time as I heal more? Or could it be something else that needs addressing?
This blog is very helpful and gives me hope. I had a lumpectomy and sentinel node biopsy 1 year ago, followed by radiation and chemotherapy. I have had armpit & upper arm pain and hypersensitivity ever since. More recently I have been experiencing sharp pain in my chest, wrapping around to the upper back, in addition to the armpit discomfort. My surgeon has said nerve damage from a sentinel node biopsy is rare… but here I am. I take neurontin only at night; it gives a little bit of relief. I also do stretches.
If no other cause of this pain is found on the chest xray (I will find out the results of that today), I will be seeking a pain management specialist. Do you happen to know someone in the Denver area who is knowledgeable about this?
Thank you so much.
Nothing found on chest xray. Which leads me to think this is nerve-related. Apologies for the detail. Thank you.
I had a hysterectomy on July 24, 2018, laparoscopic Supra cervical, uterus, both ovaries and tubes. Since surgery I have experienced muscle tightening in the left glute and pelvic muscles and left arm tightening and nerve pain under arm pit into chest wall and down inside of left arm. I have just been diagnosed with pudendal nerve pain and am in physical therapy. Do the two nerve pains go together? Odd that it all happened right after surgery. Would like to hear any advice. In a lot of pain.
My physio therapist was saying that this is probably the issue with the pain I’ve been having. I’ve had a lot of pain in my shoulder blade and she’s been trying to work on that but in the process we discovered that the pain is reflecting to my shoulder blade because I have no feeling in my underarm due to a mastectomy 4 years ago, chemotherapy, and reconstruction. Today while she was working on my underarm she noticed what we thought might be cording and while she was trying to work that out by massaging it and pulling on my arm, I felt a strong tingling sensation in my arm and that palm of my hand. I will mention this to my oncologist when I see her again in April. Thank you so much for the info. Hopefully we can get rid of this pain somehow
Hi!
I found this article to be very informative to me as well. A year ago today I was finishing up the last chemotherapy session after I was diagnosed with Hodgkin lymphoma. I am a male, about 5’11 and 26 years old. Before I was diagnosed I had a surgeon perform a biopsy. I am not sure what it was called. He went in two different ways (very close to each other) right on my upper side under my armpit and followed all the way to the center of my upper chest where the tumor was. After the procedure he mentioned he hit and bruised a bunch of nerves along the way.
Since this Biopsy I have had pain or tingling discomfort that sometimes will make me pull over on the side of the road to get out and walk around since its so uncomfortable. I have also found tight clothes to be very uncomfortable since it usually makes me rub my chest repeatedly to try help the irritated nerves (my guess). Although sometimes it is painful, most of the time its just very discomforting. I notice when i get nervous my nerves freak out and go into a panic almost instantly. My doctor has prescribed me multiple anxiety medications to help with this but im not convinced I need to be on these. When I am driving I am fine and not nervous at all, then in a second or two my nerves freaks out to the point where I need to pull over.
Overall Im just tired of every doctor telling me this is anxiety and that I need to practice yoga. I have never had problems with anxiety before this and dont understand why I would have anxiety problems after.
Do you think what you described above could work for me in anyway?
Do my symptoms match anything you may have studied before?
If so do you know anybody in the Minnesota area that could help me with this?
Thanks!
The nerves that do this are in my upper chest and next to my armpit on the front side. Could what you decribed above help me in anyway?
I am pretty sure I am having intercostobrachial nerve pain in my right armpit. It radiates from the side of my right breast though my armpit to the back of my armpit/scapula area. It is a sharp burning, numbness pain and it has prevented me from working out. I have had diagnostic tests to rule everything else out and now I need to know how to treat this. My problem is I am having difficulty finding a doctor that understand and knows how to treat this. Do you know anyone in the bay area in Northern California that treats this that you could recommend to me. I am desperate for this pain to go away so I can work out. Or do you have any suggestions on how I can treat this.
I am at my wit’s end due to the extreme discomfort of the nerve pain under my arms. I have it in both arms but predominately under right arm pit. I have to use a pillow or ice packs as a cushion under the arms or else I have severe tingling in my hands and sometimes shooting pain. At first I thought it may be a lymph node issue because I also have a feeling of swelling on my neck. I think doctors think I’m making up or exaggerating my symptoms because they I’ve had a mammogram m ultrasound and MRI which shows no swollen lymph nodes which would be compressing the nerves. Could what I am experiencing it be intercostobrachial neuralgia? Do you have any ideas of what the neck swelling could be? (Clavicle area) Could it be related?
I am at my wit’s end due to the extreme discomfort of the nerve pain under my arms. I have it in both arms but predominately under right arm pit. I have to use a pillow or ice packs as a cushion under the arms or else I have severe tingling in my hands and sometimes shooting pain. At first I thought it may be a lymph node issue because I also have a feeling of swelling on my neck. I think doctors think I’m making up or exaggerating my symptoms because they I’ve had a mammogram, ultrasound and MRI which shows no swollen lymph nodes which would be compressing the nerves. Could what I am experiencing i be intercostobrachial neuralgia? Do you have any ideas of what the neck swelling (Clavicle areal) could be? and could it at all be related to under arm swelling? (
Is there someone who can perform this diagnosis/treatment in Florida? Specifically Tallahassee or Jacksonville or even Atlanta that you can recommend?
Hello Dr.Attaman , i do have a question, Is being left handed might cause this weird pain in the left armpit, i have it for very long years and nothing relieve it , i did many tests all negative, i have read your description and i believe i do have this type of neuralgia. i would like to visit your clinic but i am from Texas, any branch or suggestion or we have to fly Washington. please advise.
thank you
M.Azzam
Last January I had a pacemaker put in due to heart failure. Since I have been getting a sharp pain in my left shoulder under my arm pit and into my side and breast. Ibuprofen helps some but also upsets my stomach if I take too much. None of the doctors address it. I think they believe it is due to my fibromyalgia. Could this happen from my pacemaker surgery? Thank you
Finally I found a site that describes what I have exactly to a tee. 6 years ago I had a second right rotator cuff surgery, from a dog pull tear. The surgeon explained he had to redo the first one sew the shredded tissue to the bone and the surgery was more complicated than he anticipated. Shortly after the surgery I began having a weird sensation way up in my armpit, then extreme pain began down my right side after PT, eventually it went into the pec area and right chest wall. I went back to the surgeon 9 times for an explanation. He kept referring me to other pain specialists who tried things but just kept sending me somewhere else. The pain was so severe in my right side that at times I could not breath, nothing helped the pain, I have been into the ER 9 times with severe pain,mostly after some therapy, with no help.. Long, long story short, in 6 years I have seen over 30 providers with various diagnoses, therapies, injections, marijuana trials,
PT, medications, ext . Everything I tried has only aggravated the pain/symptoms and drained my bank account. I have spasms/ pain/ tightness throughout the right chest wall/ armpit up into the neck and face at times, 24/7 now. There is no one here in PA who can figure this out. I was told by a pain specialist recently at Penn Med. that it was probably a nerve stretched out and damaged during the shoulder surgery, which I had long suspected. I have had 3 nerve blocks, not sure if they helped and am due for a 4th. Thank you for putting an exact description to what is going on with me here. It fits all the symptoms perfectly, even though I have not had breast cancer surgery, I feel it is similar. I am still suffering with no help after 6 years, fed up with meds that only aggravate the condition and being passed along or dropped. I do know any stretching and most meds prescribed aggravate the condition immensely. At this point I am ready to think outside the box with herbs , supplements and oils as the medical community has failed me.
Of course your practice is too far for me to make an appointment, but if by chance you know a specialist familiar with this condition in PA, I would appreciate it. Again thank you for putting a name to this horrible debilitating long term condition at last. No on has diagnosed or helped me with it sadly most likely because it was surgical issue and never addressed. LMG
Do you k ow anyone in Canada that specializes like yourself. ( Ontario specifically)
Thank you for posting this info Dr. Attaman,
I know you can’t diagnose over the internet but I wonder if you’ve heard of this.
I have “severe” osteoporosis and for about six months I have burning, spasmodic pain radiating from my thoracic spine around my back to under my arms. I wonder if my spine could be pressing on my nerves.
Thanks for whatever info and/or advice you can give me. I would come for an appointment but I’m in Vermont, rather far away.
Nancy O’Brien
Ive had this come stay and go since about 2007 I get a sharp and doll tingle stabbing pains in my armpits and breasts but mostly on yhe left side , I also have sciatica on my right side but will sometimes be on the left , I also get pain that goes from my neck and base of back to the middle of my back , please help how can I get my doctors to listen to me ,
I have pain on the right side of my breast under my arm. You can tell there is inflammation on that side of my body. I had a mammogram and it is not breast related. Could this be related to nerves?