A rarer cause of chronic pelvic and genital pain is a disease called Pudendal Neuralgia. I have treated many patients over the past few years with this diagnosis, and it has been professionally rewarding for me – and a long-overdue relief for them.
My offices are in Bellevue and Seattle, WA, but I have helped pudendal neuralgia sufferers from all over the world and the US, including patients from California, Oregon, Idaho, British Columbia, New York, Texas, Georgia, South Carolina, Montana, Arizona, Nevada, Utah, Kansas, Michigan, Alaska, Hawaii, London, and Ecuador. I may be able to help you, too.
Suffering from pudendal neuralgia? Call my office at 206-395-4422 (Seattle) or 425-247-3359 (Bellevue), or email us, or schedule an appointment online.
What Is Pudendal Neuralgia?
What Causes Pudendal Neuralgia?
Synonyms of Pudendal Neuralgia
Conditions Related to (But Different From) Pudendal Neuralgia
Pudendal Neuralgia in Women
Pudendal Neuralgia In Men
Pudendal Neuralgia Following Pelvic Surgery
Pudendal Neuralgia in Young People
Pudendal Neuralgia in Older People
Diagnosing Pudendal Neuralgia
How to Treat Pudendal Neuralgia
Pudendal Neuralgia Treatment Options
What Is Pudendal Neuralgia?
From the Health Organization for Pudendal Education:
“Pudendal neuralgia is a commonly overlooked condition when evaluating chronic pelvic and genital pain disorders. The pain associated with many of the following disorders may be caused by (or in part by) pudendal neuralgia or pudendal nerve entrapment: vulvodynia, vulvar vestibulitis, interstitial cystitis, irritable bowel syndrome, chronic or non-bacterial prostatitis, prostadynia, burning scrotal syndrome, chronic pelvic pain syndrome, proctalgia fugax, hemorrhoids, coccydynia, piriformis syndrome, anorectal neuralgia, pelvic congestion, pelvic floor dysfunction, ischial bursitis, levator ani syndrome, and others. All of these disorders can have the same symptoms as pudendal neuralgia or actually be caused by PN. Sadly, it is common for patients with any of these conditions to be told their problem is psychosomatic and to seek psychiatric help.” — Health Organization for Pudendal Education
What Causes Pudendal Neuralgia?
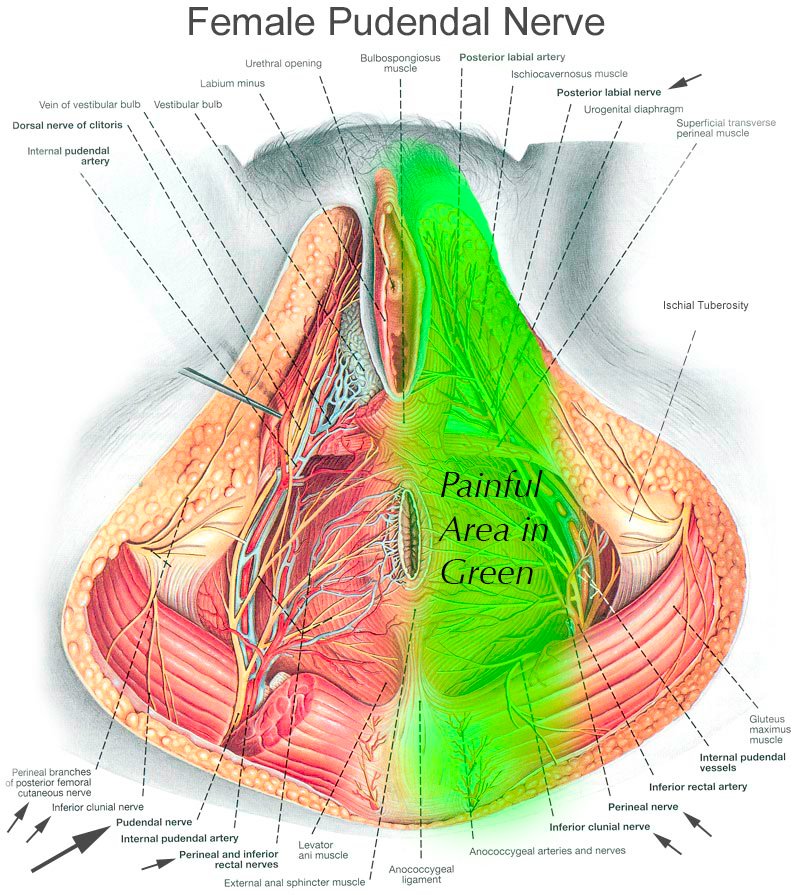
The pudendal nerve is a very little-known but very important nerve in the pelvis. It is a nerve that provides sensation to your inner buttocks, anus, perineum (the area between your anus and genitalia), and genitals.
This nerve can be injured or irritated for many reasons. In roughly 50% of patients, we have no idea what triggered the issue. Some patients have Pudendal neuralgia from falling on their buttocks while snowboarding. It can be as simple as that. Some patients have endured serious surgeries such as pelvic sling mesh placement and have woken up with this pain. Regardless of the cause, the symptoms can be severely debilitating.
Synonyms of Pudendal Neuralgia
Many people who experience pudendal neuralgia haven’t heard of it, or don’t know it by that name. There are many other ways to refer to the condition, precisely or generally. Other terms that may refer to pudendal neuralgia include: pudendal nerve pain, pudendal nerve entrapment, pudendal nerve irritation, pudendal neuropathy, pelvic nerve pain, pelvic nerve entrapment, perineal pain, perineal nerve pain, pudendal canal pain, ischiocavernosus pain, Alcock’s syndrome, Alcock’s canal syndrome, or cyclist’s syndrome, numb penis, scrotum nerve pain, anal nerve pain, vagina nerve pain, penis nerve injury, chronic pelvic pain syndrome (CPPS), dorsal penile nerve pain, dorsal penile nerve pain syndrome, and dorsal nerve compression syndrome (DNCS)
Conditions Related to (But Different From) Pudendal Neuralgia
Other conditions may feel like pudendal neuralgia, share symptoms with it, or be mistaken for it or misdiagnosed as it. Conditions that are NOT the same as pudendal neuralgia include: genitofemoral neuralgia, ilioinguinal neuralgia, posterior femoral cutaneous neuralgia, prostate pain, endometriosis, endometrial pain, and persistent genital arousal disorder (PGAD).
In experiencing pudendal neuralgia you may also experience pain with orgasm, pain with ejaculation, vagisismus, or erectile dysfunction.
Pudendal Neuralgia In Women
Typically my female patients with pudendal neuralgia experience severe perineal burning electrical pain and pain around the genitals, especially the vulva and the clitoris. They often complain of a sensation of “sitting on a rock” near their sitting bones (ischial tuberosities). Women very commonly have pain around the rectum, perineum (area between the anus and vagina), vagina, and upper inner thighs. Some may have pain around the lower abdomen as well.
We find approximately 50% of women develop pudendal neuralgia after abdominal or pelvic floor surgery or childbirth. The remainder have an unknown cause.
Pudendal Neuralgia In Men
Men with pudendal neuralgia typically have pain more focused around the scrotum or end of the penis.
Some men have a very specific cause of pudendal neuralgia, such as sports-related injures – particularly bicycling – or trauma to the pelvis during activity. The majority of cases, however, have no specific known cause. That can be very frustrating because such men may be left wondering “what went wrong?” for a long time. Men very commonly have pain around the perineum, scrotum, and very commonly in the glans penis (tip of the penis).
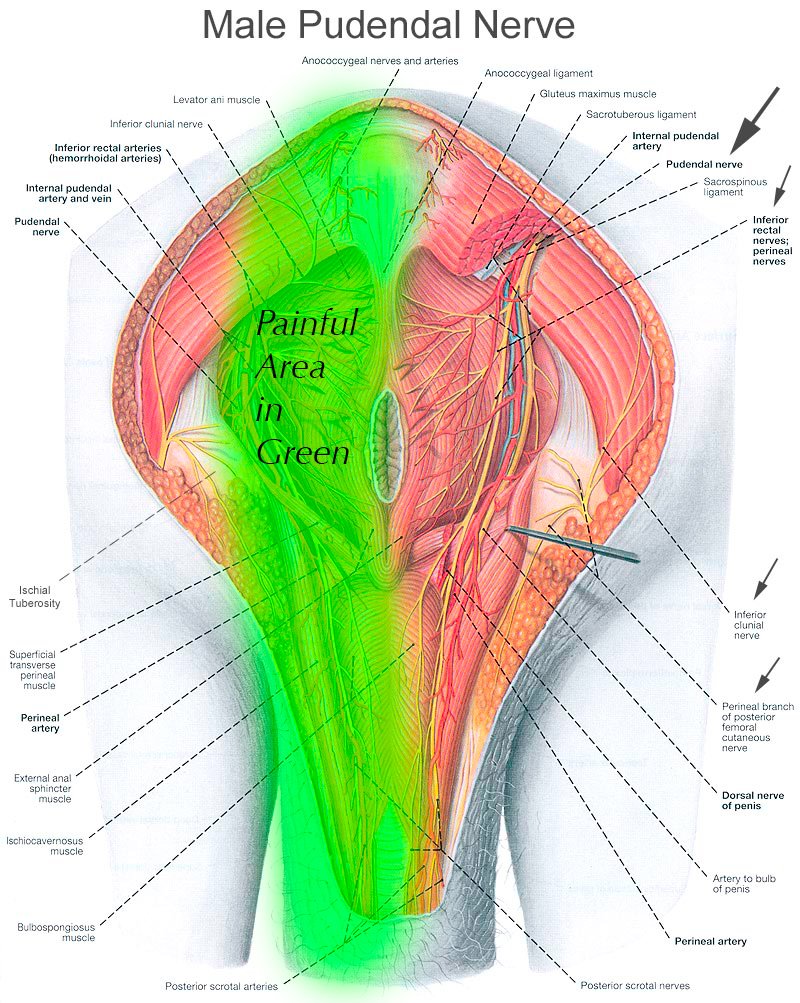
The images you see demonstrate the course of the pudendal nerve, and you can imagine that burning, electrical, stinging pain anywhere along this nerve would be extremely distressing.
Pudendal Neuralgia Following Pelvic Surgery
Pelvic floor surgery often triggers pudendal neuralgia. For women, pelvic floor surgery, sling surgery, endometriosis surgery, or even abdominal surgery (often for endometriosis) can cause pudendal neuralgia. For men, prostate surgery, radiation therapy, or even biopsy can cause pudendal neuralgia.
Pudendal Neuralgia in Young People
Young men very commonly have pain around the perineum, scrotum, and very commonly in the glans penis (tip of the penis). Some young men have a very specific cause of pudendal neuralgia, such as sports related injures (bicycling is the most common), or trauma to the pelvis during activity. Many young men have incurred it after sexual trauma (physically aggressive masterbation is a very common cause). Another common cause in young men is untreated anxiety or panic disorder. This causes men to clench and tense their pelvic floor muscles chronically, which results in overdevelopment (hypertrophy) of the pelvic floor muscles. In particular, the obturator internus muscle is frequently up to double the size of normal in such young men. This compresses Alcock’s canal and the pudendal nerve which passes through it. Thus, biofeedback is often used in conjunction with our specialized injection procedures such as botox to help such men relax their pelvic floor muscles.
We find approximately 50% of young women develop pudendal neuralgia from abdominal or pelvic floor surgery or childbirth. Undiagnosed endometriosis is also a common cause. The remainder have an unknown cause. Young women very commonly have pain around the rectum, perineum (area between the anus and vagina), vagina and upper inner thighs. Some have pain around the lower abdomen as well.
Pudendal Neuralgia in Older People
Same as for men and women. The exception is older men who have had prostate surgery often develop it. “If you have had prostate surgery or radiation treatment, pudendal neuralgia can often develop as a result.” Also for both sexes “if you have had hemmorhoid surgery, this can trigger pudendal neuralgia as well”
Diagnosing Pudendal Neuralgia
Establishing a diagnosis of pudendal neuralgia can be a long and winding road of appointments, tests, misdiagnoses, and surprises. The majority of people with pudendal neuralgia have suffered from it for years before even learning what it is.
Diagnosing pudendal neuralgia is complex. If you are reading this page, chances are you’ve already been seen by multiple specialists.
If you are a woman, a gyenecologist or urogynecologist is a common specialist to consult. If you are a man, you may have seen a urologist or neurologist. Whom you consulted with is important, because most cases of pelvic pain are not the result pudendal neuralgia, and can be discovered by those kinds of specialists.
However, when the specialists you have seen are unable to find anything wrong to explain your symptoms, a diagnosis of pudendal neuralgia is much more likely. The diagnosis can be confirmed by the following methods:
1) We can use ultrasound to visualize your pudendal nerve and inject strong numbing medicine around it. If that results in complete or near-complete relief of your pain for a few hours, we can confirm a diagnosis of pudendal neuralgia.
2) We can use ultrasound to place a specialized needle near the pudendal nerve, and then pass a very mild electric signal through the nerve. This will “light up” your nerve and you will feel a buzzing sensation along the entire course of the pudendal nerve. If this matches or is “concordant” with your typical symptoms, we can confirm the diagnosis.
Many ask whether nerve-conduction study tests are required, and the answer is generally no, they are not An abnormal nerve conduction study does not mean pain is coming from the pudendal nerve. For example, one may have an abnormal nerve conduction study and have no pudendal nerve symptoms. The same is true of specialized MR studies such as MR neurography; I’ve had many patients with completely normal MR neurography studies but who have complete resolution of their symptoms from pudendal nerve blocks or stimulation. MR neurography and nerve conduction studies can be helpful in surgical planning and workup, if surgery is ultimately required, but that is relatively rare.
How to Treat Pudendal Neuralgia
The first step in treating pudendal neuralgia is education. This means finding physicians that know the nerve. Unfortunately, there are very few of us. This seems to be due to the fact that we are not taught about the pudendal nerve in medical school, residency, or even fellowship training. Indeed, I’ve spoken to urologists and gynecologists who either had forgotten about this nerve or had no idea it can play a role in chronic pain. Even though I completed a very intensive Pain Medicine fellowship, I never learned of it either. It was not until I started seeing patients in my clinic for whom nobody had found a diagnosis that I did further research and came to appreciate the importance of this nerve.
I’d strongly recommend you visit pudendalhope.info to get educated on this condition. It is a wonderful resource for education and resources.
The next step is getting diagnosed and treated. Typically, this means seeing a urologist, uro-gynecologist, or OB/GYN specialist who likes to treat pelvic pain. One such person I can highly recommend in my state of Washington is Dr. Cindy Mosbrucker and her colleague Dr. Irene Grias. If it is found that your pain is not due to issues with your internal organs, then the pain may be due to pudendal neuralgia. This is when I can help.
Typically I will review your records from the other specialists you have seen to be sure no diagnosis has been overlooked. I review any tests such as MRIs you may have had. I then perform a very careful history and gentle physical exam. We then discuss treatment options.
Pudendal Neuralgia Treatment Options
Treatment options for pudendal neuralgia are generally “multi-modal,” which means it would involve referral to various specialists with unique skills in treating this issue, such as physical therapists who work on the pelvic floor. Medications such as custom made suppositories to relax your pelvic nerves and muscles may be prescribed. Special Imaging studies such as MRI neurogram of the pudendal nerves may be ordered. Typically, I will want to confirm your Pudendal nerves are causing your pain by using an ultrasound machine to see the nerves and guide a thin needle to them through your buttocks and turn them off temporarily via a local anesthetic injection. This is called an ultrasound-guided pudendal nerve block. Oftentimes the treatment just detailed is sufficient to cure the issue. If insufficient, you may be a candidate for other procedures I perform, such as low volume caudal epidural injections, pulsed radiofrequency ablation of the pudendal nerves, or spinal cord stimulation trial over a special area of the spinal cord called the conus meddularis.
Need to discuss options? Contact me
Pudendal Neuralgia is a challenging condition to treat and to diagnose, but there is hope. Feel free to contact me, Dr. Jason Attaman, to discuss treatment options. You can call my office at 206-395-4422 (Seattle) or 425-247-3359 (Bellevue), or to schedule an appointment online.
